An innovative team approach to improving mobility and preventing fractures
A multidisciplinary group of UC Davis Health geriatric, orthopedic surgery, endocrinology and rheumatology clinicians have formed a new Fragility Fracture Program. The goal is to provide comprehensive treatment and prevent more fractures among those most at risk due to low bone density and other factors.
The new program falls under UC Davis Health’s new Healthy Aging Clinic, a one-stop shop that serves patients and their caregivers, offering integrated specialty clinical care and services.

Improving mobility to prevent falls
A key aspect of the Fragility Fracture Program is a focus on mobility.
“We take a geriatric approach with our mobility clinic,” said Alia Tuqan, a board-certified geriatrician and interim medical director of the clinic. “We start with a physical exam to assess their risks for an additional fall, then work with the patient and caregivers to formulate a plan to prevent another fall.”
Clinic nurse practitioners run the mobility program. During the exams, they evaluate a patient's vision, neuropathy, orthostatics, cognitive impairment and any medicines that could increase the person’s risk of falling.
Measuring gait: the sixth vital sign
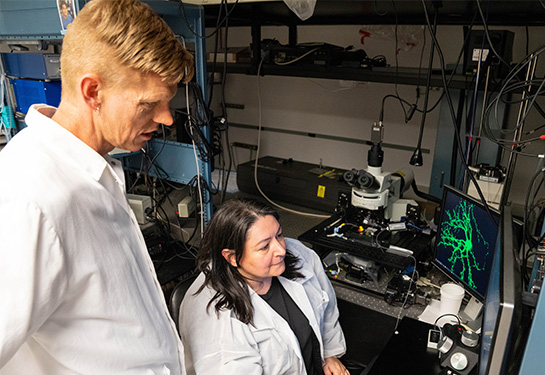
While clinicians observe mobility in the clinic, UC Davis Health researchers are in the Biomechanics, Rehabilitation, and Integrative Neuroscience (BRaIN) Lab studying how to better detect the subtle yet vital changes in walking patterns.
“Walking is such an important marker of physical health and function. People have often named it a sixth vital sign,” said Carolynn Patten, professor and director of the BRaIN Lab in the School of Medicine Department of Physical Medicine and Rehabilitation. “By analyzing the variability and characteristics of gait parameters, such as stride time, we can predict falls, detect cognitive decline, and map certain parameters to specific forms of dementia or mild cognitive impairment.”
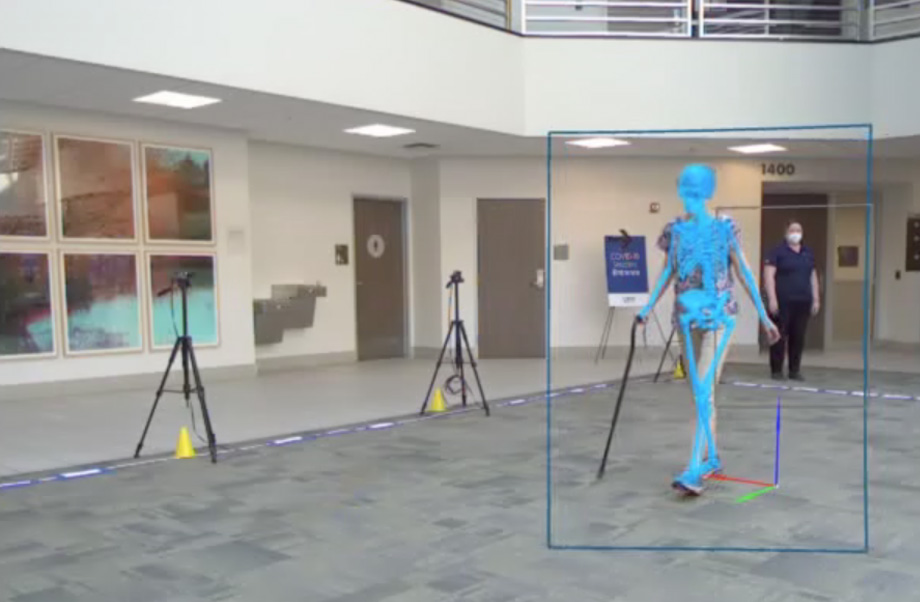
UC Davis Health clinicians assess gait using an innovative project called Walking in the Living Domain (WILD). It uses markerless motion capture technology to enable comprehensive 3D gait analysis for a patient outside the laboratory, using a set of eight cameras in health facilities and community settings.
A multidisciplinary approach to a broken bone
Fragility fractures are one of the more common breaks in patients with low bone density, and result from a fall from a standing height or less.
“Fragility fractures, which most commonly occur at the hip, spine or wrist, are an indication that the body’s bones have been weakened by an underlying condition,” explained Hai Le, assistant professor of orthopaedic surgery. “Therefore, the patient at the highest risk of a fragility fracture is someone who has just had one.”
A recent study by Le and his team found that patients who have had a fragility fracture are more likely to experience another one in the future. It also highlighted the lack of follow-up care to prevent additional fractures. The researchers suggested cases of osteoporosis, a condition where bones become weak and brittle, should be treated earlier.
“When patients experience fragility fractures that require surgery, it is our job to get those patients back on their feet, but we are not the experts on preventing the next fracture,” Le said. “That's when we bring in our colleagues from endocrinology and rheumatology who are the experts in diagnosing and treating osteoporosis or other illnesses related to low bone density.”
Diagnosing and treating osteoporosis early
“My role in diagnosing osteoporosis includes conducting a complete laboratory screening of potential risk factors from a hormonal standpoint,” explained Polly Teng, assistant professor of endocrinology and orthopaedic surgery.
Some laboratory tests include a patient’s vitamin D, calcium, and parathyroid and thyroid hormone levels, all of which can affect bone fragility.
“These treatments can help manage the underlying causes of a patient’s bone fragility, improve bone stability, and prevent future fractures,” said Barton L. Wise, associate professor of rheumatology and orthopaedic surgery. “There are many good medications to treat illnesses that affect bone density. Diagnosing our patients properly allows us to identify the best care plan for each patient and evaluate if they have any other underlying disorders.”
Patients also receive visits from nutritionists who provide dietary guidance and physical therapists who lead them through exercises to strengthen supporting muscles and improve balance and mobility.
Eyeing national impact
Increased preventive treatment programs like UC Davis Health’s Fragility Fracture Program could have a major impact on public health costs in the United States. The National Osteoporosis Foundation reported that approximately 1.8 million Medicare beneficiaries suffered about 2.1 million osteoporotic fractures in 2016.
“If we could reduce secondary fracture development by just 20%, we could save Medicare over one billion dollars annually,” Le said. “Comprehensive fracture programs could improve patient outcomes and provide our Medicare system additional resources to support other programs.”