If anything comes close to the anguish accompanying the news that a child has cancer, it's the agony of waiting for a precise diagnosis – and the start of treatment to attack that disease. At UC Davis, oncologists meet every day with families struggling with such circumstances. And they are working in earnest to ease their distress.
In a laboratory near the UC Davis Cancer Center, researchers are striving to develop a quick and reliable diagnostic technique to identify all types of cancer from a small blood sample.
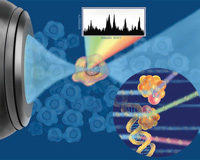
Ultimately, they hope their technology – based on a new application of Raman spectroscopy – could help doctors choose the most suitable drug for a particular cancer and assess the effectiveness of treatment within hours or days.
The work is in the early stages, and the scientists caution that many possible stumbling blocks stand in their way. But if they achieve their goal, cancer patients could get answers – and treatment – far more quickly than they do today.
"Making diagnoses now is not always the simplest process on the planet, despite what you see on TV," says pediatric oncologist Douglas Taylor, one of two faculty members leading the research. "It involves often archaic technologies and multiple technicians. And it can often take days or occasionally weeks to figure out exactly what type of malignancy someone has."
Taylor has teamed up with physicist Thomas Huser to make his cancer-diagnostic machine a reality. They are developing a novel application of a technique called laser tweezers Raman spectroscopy. The breakthrough application involves using laser beams to hold floating cells in place, measuring the light scattered by their nuclei and, based on these measurements, accurately identifying them as cancer cells.
In January 2006, Taylor, Huser and their colleagues published a paper in the Biophysical Journal showing that they could use the technology to distinguish normal white blood cells from cells taken from leukemia cell lines used in cancer research. Since then, they have successfully repeated those experiments using cells taken from actual leukemia patients.
"Each type of cell has its own biomolecular signature and we were able to use that to distinguish the cancer cells from the normal ones," Taylor explains. Publication of these newer results is pending.
The unique collaboration between Taylor and Huser was made possible by the Center for Biophotonics Science and Technology, a National Science Foundation facility based at UC Davis. Formerly employed at Lawrence Livermore National Laboratory, Huser now serves as chief scientist for the center and is a UC Davis associate professor in the Department of Internal Medicine. Taylor is director of the UC Davis pediatric stem-cell transplant program and an associate professor of pediatrics.
The center's goal is to spawn partnerships that lead to the application of the physical sciences to medical problems. In this case, the problem is the need for a better, faster and cheaper method for diagnosing cancer. Despite numerous advances in the treatment of cancer, the cornerstone of modern cancer screening is a method developed in the late 1800s. And not all cancers can be identified by the fastest current method, flow cytometry, Taylor says.
The technology behind laser tweezers Raman spectroscopy is not new. Raman spectroscopy was invented in the 1920s, while laser trapping of cells was first developed about a quarter-century ago. It wasn't until spectroscopy could be fine-tuned and lasers became smaller, less expensive and more precise that these technologies could be applied to biological samples.
"The marriage of the two technologies only happened in the last five to six years," Huser says. "Now we can use lasers to optically suspend a cell within the laser focus and then determine its chemical signature."
The amount of laser light that is scattered by the nucleus of a cell depends on the amount and configuration of the biomolecular compounds it contains, such as DNA, RNA and proteins. More specifically, the number, density and type of molecular bonds determine the shift in the wavelength of the scattered light. Although minute, these differences are measurable and so unique that each cell type has its own spectroscopic fingerprint, Huser says.
Using these biomolecular fingerprints to find and define cancer in a blood sample, or elsewhere, would be a huge improvement over many current screening methods. Some diagnostic tests, for example, require patients to ingest radioactive materials and undergo CT scans. All the while, patients and their families are waiting – and worrying.
"I think the most distressing part is the waiting, because until the complete problem is known, the complete solution cannot be discussed," Taylor says. "Once the cancer is identified, and folks are marching toward a solution, there's security in that, and an element of solace."
Huser predicts that it will take four to five years for the team to show that the technology is not only safe and effective for widespread use as a diagnostic tool, but also faster than current methods.
"We have shown that Raman spectroscopy works to distinguish cancer cells," Huser says. "Now we just need to show that we can do it ten thousand times faster. At that point, it becomes interesting."
The group's ongoing experiments include automating the technology. They are working toward developing a high-throughput instrument and exploring other applications that promise advancements in patient care.
"In the future, we hope not only to screen for the presence of cancer, but also to quickly determine whether patients are responding to treatment and detect residual disease," Taylor says. "That's the diagnostic nirvana."
As a physician treating leukemia patients, Taylor's biggest hope is to one day use laser-trapping Raman spectroscopy technology to remove cancer cells from a patient's blood and then return the disease-free blood to that patient. While this and the other applications remain at best a distant reality, "in theory, the technology lends itself to these possibilities," Taylor says.
At UC Davis Children's Hospital, Medical Director Anthony Philipps is cheering on his colleagues' work, and waiting hopefully. When it comes to cancer diagnosis, he says, time is of the essence, and Raman spectroscopy could vault the process forward.
"If so, that will mean we can determine a course of treatment quicker, and that's beneficial to the patient," says Philipps, who is also the chair of pediatrics.
In the short-term, Philipps already sees a payoff. By bringing together physical scientists from the Livermore lab and UC Davis physicians, the project has created a fertile environment for collaboration that can only benefit cancer patients.
"It's fun to see it happen," says Philipps, who anticipates more collaboration in the future. "We knew it was going to work. But still, it's great to see the results."