Discovery through synergy
Biotechnologies combine to improve cancer detection
We are slowly gaining ground on cancer. Targeted treatments, like Herceptin against breast cancer, have been remarkably successful. New approaches to immunotherapy also are showing great promise. However, the best treatments in the world may not be good enough if the disease is not detected early. Cancer is a disease of mutations, and the longer it goes undiscovered, the more mutations it can develop — variations that can make tumors resistant to treatment.
Both researchers and clinicians recognize this problem and are working hard to solve it. At the National Cancer Institute-designated UC Davis Comprehensive Cancer Center, scientists are building a new class of scanners, as well as developing new imaging agents that will shine a light on hidden cancers. These technologies could help detect cancers when they’re smaller and easier to treat.
Before cancer can be treated, it must be detected. The earlier cancers can be detected, the better the patient’s prognosis. That’s where imaging comes in.
The promise of PET
For more than 30 years, positron emission tomography (PET) has been a powerful tool to detect cancer. The technology is relatively simple; a radioactive tracer is attached to a molecule, such as a sugar, and injected into a patient. Because cancers are hungry and like to eat sugar, the molecule and its radio-active partner concentrate in those tumors. The scanner then picks up the radiation concentrations, detecting the cancer.
It’s good technology, but Ramsey Badawi, director of nuclear medicine research, thinks it can be better.
“Current PET scanners only cover 15 to 20 centimeters at a time,” says Badawi. “That means we can only image a small portion of the body at any one time, which slows the process and wastes radiation. However, if we build a scanner that’s two meters long, we will see everything all at once, including smaller tumors. This will be great for patients, because it will work faster, require less radiation and detect cancer at its earliest stages.”
The National Cancer Institute (NCI) has awarded Badawi a prestigious “Provocative Questions” grant to develop the technology. Of 700 applications, his project was one of only 57 to receive funding. The Badawi group is working with colleagues at Lawrence Berkeley National Laboratory, the University of Iowa and the University of Pennsylvania to make this happen.
A crush of data
Building such a large scanner brings a host of technical challenges. For example, with radiation coming from diverse angles, images can get blurred. Sophisticated software must be developed to determine where in the body the radiation originated and where it ended up.
The most significant challenge is the amount of data that will enter the scanner at once — not gigabytes, but terabytes. The researchers are taking their inspiration from websites like Facebook and Google, which use algorithms to instantly sort huge amounts of information. Badawi and his team are using similar algorithms and adjusting them to meet the large scanner’s huge data-sorting needs. Better infor-mation-handling translates into sharper images.
A shopping list of benefits
The new scanner will be 30- to 50-times more sensitive than current scanners, allowing clinicians to detect tumors at their earliest stages. This added sensitivity brings other benefits. Scans can be completed in seconds, which is particularly helpful when imaging children.
Because of the scanner’s increased sensitivity and speed, patients will require less radiation, allowing researchers to conduct studies they can only dream of now. If less radiation is used, physicians can use PET to scan high-risk patients before they develop symptoms. Volunteer study participants can also be safely scanned to study inflammation, obesity, even gut bacteria.
Seeing-eye molecules
While Badawi’s team works to build a better scanner, Julie Sutcliffe and her team are working with Siemens to develop better tracers. PET scanning for cancer patients typically involves use of tracers inserted into the body. Current tracers generally combine glucose (a sugar) with radioactive fluorine (a chemical element). Since most tumors take up sugar at a higher rate than normal cells, they will light up on PET scans. The problem is that these tracers also light up the heart and brain, which can muddy the picture and make diagnosis more difficult. That can muddy the picture and make diagnosis more difficult. Sutcliffe’s group is developing new tracers that more precisely target cancers.
“Different cancers often have different biomarkers, and we’re trying to target those biomarkers, much in the same way Herceptin targets HER2-positive cancer,” says Sutcliffe. “We can do the same with an imaging agent. We can put the imaging agent onto a targeting molecule and it will light up in the areas that have that biomarker.”
Sutcliffe’s team is working with cell-surface proteins called integrins, prevalent in cancer cells, particularly metastatic ones. They are identifying molecules that will seek out these receptors and bring the radioactive payload with them. Specifically, they are interested in agents that will precisely target breast and pancreatic cancers. Breast cancer affects millions of women, while pancreatic cancer exhibits few symptoms and is notoriously difficult to detect.
In addition, a tumor-seeking molecule could do more than guide radiation particles to cancers; it could also guide treatments.
“Our long-term goal is to develop an imaging agent and a therapeutic at the same time,” says Sutcliffe.
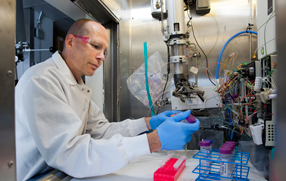
It’s hard work. First, research using radioactive materials requires appropriate precautions. Second, the isotopes have very brief half-lives, in some cases just a few minutes. Scientists can’t use normal slow chemistry to attach the isotope to the targeting agent because they simply don’t have the time.
“It’s a difficult challenge,” says Sutcliffe. “We’re using everything from our chemistry toolkit to make this work.”
The big payoff
One of the biggest hurdles in developing new cancer therapies is that many drugs fail late in the process. By that time, hundreds of millions of dollars have been invested. Both Badawi and Sutcliffe believe the technologies they are developing could profoundly improve this process, eliminating poorly performing drugs earlier in the pipeline.
“The earlier you can winnow out the bad ones, the more resources you can concentrate on the good ones,” says Badawi. “Better PET technology could help us winnow out inferior drugs.”
More sensitive scanning could allow researchers to measure where a drug goes in the body and how long it stays there. The scanner’s enhanced sensitivity would also allow researchers to test compounds that would be toxic in larger amounts. A drug found to be toxic to the heart would be removed from the pipeline.
“You can attach any number of drugs with radioactive tags and find out what a drug does,” Badawi says. “Does it go to the cancer, does it do bad things like go to the bone marrow or hang around in the liver too long? If you can do that, you can say ahead of time that it’s probably going to be pretty toxic and move along to the next drug.”