Bits & pieces
New technologies rolled out for prostate, bladder cancer surgeries
The UC Davis Department of Urology is the first in the region to use two new technologies to improve care and outcomes for prostate and bladder cancer patients.
The technologies are fluorescence cystoscopy, also called blue light cystoscopy, to enhance surgery for bladder tumor removal, and fusion-guided biopsy to more precisely target treatment areas for prostate cancer patients.

Marc Dall’Era, associate professor and vice chair of the Department of Urology, said the fluorescence cystoscopy “helps us better visualize small tumors that may not be identified under white light. The blue light also helps the surgeon see the edges of the tumor to enable a more complete surgical removal of the tumor.”
The thorough view and removal of bladder tumors mean there is a decreased risk of cancer recurrence. The American Urological Association has added fluorescence cystoscopy to their recommended guidelines for treating bladder cancer.
The fusion-guided biopsies blend MRI and ultrasound for better prostate cancer detection. After an MRI, a radiologist circles suspicious areas before the image is uploaded to a biopsy machine. The urologist then performs an ultrasound and biopsy. The MRI image is overlaid on the ultrasound image, which is done in real time, to help the urologist target a specific area for biopsy.
“It’s drastically changed the way we are diagnosing and treating localized prostate cancer,” said Dall’Era, adding that the approach is especially beneficial to patients under active surveillance who have lower-risk tumors.
Hepatitis B and Liver Cancer
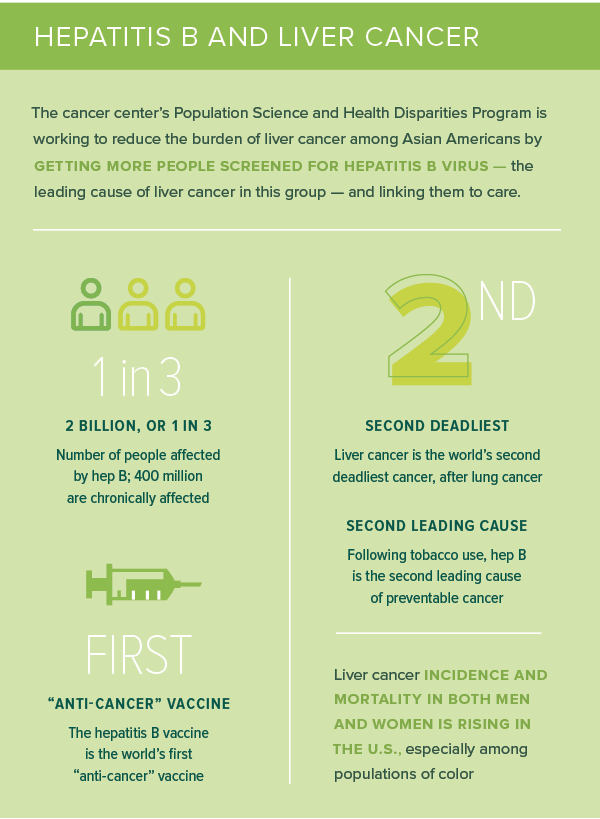
The cancer center’s Population Science and Health Disparities Program is working to reduce the burden of liver cancer among Asian Americans by getting more people screened for hepatitis B virus — the leading cause of liver cancer in this group — and linking them to care.
- 2 billion, or 1 in 3 - Number of people affected by hep B; 400 million are chronically affected.
- The hepatitis B vaccine is the world’s first “anti-cancer” vaccine.
- Liver cancer is the world’s second deadliest cancer, after lung cancer.
- Following tobacco use, hep B is the second leading cause of preventable cancer.
- Liver cancer incidence and mortality in both men and women is rising in the U.S., especially among populations of color
De Vere White endowment to help young science students
Ralph de Vere White, who stepped down in June after serving 20 years as the cancer center’s director, has been honored with an educational endowment in his name.
The Ralph de Vere White Endowed Education Fund was created by his wife, Antoinette, for the purpose of training the next generation of medical professionals who will continue the fight against cancer. She hopes to reach a target of $200,000.
The fund will be used to support undergraduate and high school students who plan to participate in cancer research training programs or need funds to conduct summer research, attend conferences or take admissions exams.
The fund will be available only to students who have demonstrated a special aptitude for the study of cancer science, and it will give special preference to individuals with personal perspectives on issues facing marginalized communities.
To learn more or to donate visit ucdmc.ucdavis.edu/cancer/DVW.endowment
Breast cancer
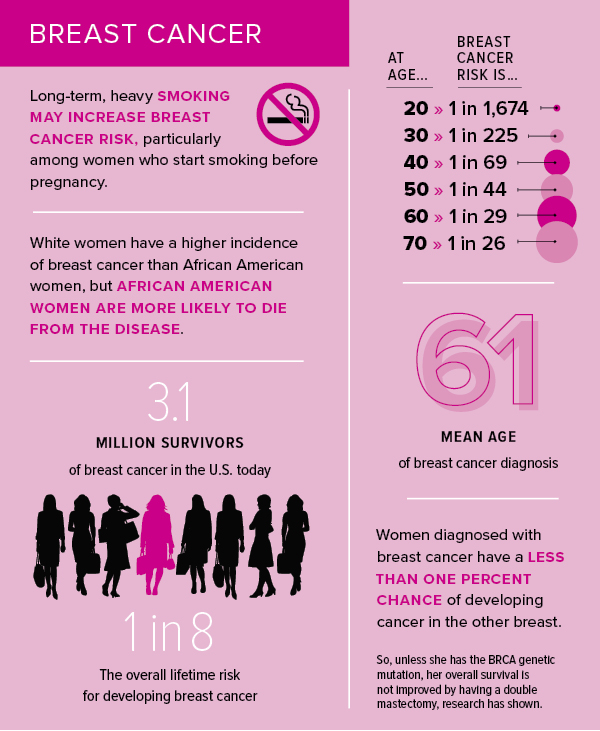
- Long-term, heavy smoking may increase breast cancer risk, particularly among women who start smoking before pregnancy.
- White women have a higher incidence of breast cancer than African American women, but African American women are more likely to die from the disease.
- 3.1 million survivors of breast cancer in the U.S. today
- 1 in 8 overall lifetime risk for developing breast cancer
- At age 20, breast cancer risk is 1 in 1,674; at 30, 1 in 225; at 40, 1 in 69; at 50, 1 in 44, at 60, 1 in 29; at 70, 1 in 26
- mean age of breast cancer diagnosis is 61
- Women diagnosed with breast cancer have a less than one percent chance of developing cancer in the other breast.
- So, unless she has the BRCA genetic mutation, her overall survival is not improved by having a double mastectomy, research has shown.
Sources: American Cancer Society, American Society of Breast Surgeons website – breastsurgeons.org, Breast Cancer Facts and Figures 2015-2016 – breastcancer.org, Smigal C, Jemal A, Ward E, et al. Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin. May-Jun 2006;56(3):168-183.
Lay educators help boost colorectal screening rates in Hmong
A study by Elisa Tong, associate professor of internal medicine, found that Hmong Americans are more likely to understand the importance of colorectal cancer screening and get screened when they get information from specially trained Hmong lay health educators.

The study, published in the journal Cancer, was conducted in collaboration with the Hmong Women’s Heritage Association in Sacramento, home to the third largest Hmong population in the U.S. This group is disproportionately affected by high rates of poverty and other socio-economic challenges that affect preventive health screening rates.
“Hmong Americans in the age group for colorectal cancer screening are especially vulnerable because of low levels of education and limited literacy, even in the Hmong written language,” said Tong. “Added to that are the cultural barriers that can come with receiving Western medical care.”
Penny Lo, project coordinator with the Hmong Women’s Heritage Association and a study co-author, said the study opened doors to introducing cancer prevention education to the Hmong community.
“Lay health educators have access to the community because of family or church relations that even nonprofit organizations can’t normally reach,” she said.
Hybrid treatment hunts down and kills leukemia cells
UC Davis pediatric cancer researcher Noriko Satake, in collaboration with Ionis Pharmaceuticals, has developed a hybrid treatment for B-cell type acute lymphoblastic leukemia (ALL) that shows promise in mice.
The treatment, which harnesses a monoclonal antibody to deliver single-strand (antisense) DNA to ALL cells, reduces levels of a certain protein that helps cancer cells survive. Importantly, the treatment also limits damage to other tissues.

“This could be a new type of treatment that kills leukemia cells with few side effects,” said Satake, associate professor in the Department of Pediatrics.
ALL is a disease of the bone marrow and the most common type of childhood cancer. While most children survive ALL, many suffer late or long-term side effects from treatment, which may include heart problems, growth and development delays, secondary cancers and infertility.
The hybrid treatment was effective against ALL cell lines grown in the laboratory and in a mouse model. Animals that received the hybrid therapy survived significantly longer than those in the control group.
Satake’s work was supported by The Hartwell Foundation, Keaton Raphael Memorial Foundation, National Center for Advancing Translational Sciences, the California Institute for Regenerative Medicine, National Institutes of Health and a UC Davis Comprehensive Cancer Center Support Grant.
Key tips from our oncology dieticians

- Add a colorful mixture of fresh fruits and vegetables to your diet
- Balance your healthy diet with favorite activities that minimize stress and support a positive outlook
- Minimize your intake of alcohol
- Limit your fried food and simple sugar consumption
- Eating well after a cancer diagnosis helps you feel better, keep your strength and energy up, tolerate treatment better, lower risk of infection and support healing and recovery
- Include healthy fats like avocado, olives, nuts and seeds
- Ask to meet with an oncology dietitian if you are confused or overwhelmed by conflicting nutritional advice
Precious time for the great-grandchildren: Lymphoma patient celebrates 100th chemo treatment
When Barbara Mooney was diagnosed with non-Hodgkin’s lymphoma in 1999, she didn’t think she would see her grandkids grow up. She was wrong.
The journey has been one of great triumph for the 75-year-old native New Yorker, thanks to the innovative care she receives at the UC Davis Comprehensive Cancer Center.
After finishing her chemotherapy regimen in 2001 she moved to Elk Grove, Calif. to be closer to her family and came under the care of Joseph Tuscano, a hematologist-oncologist at UC Davis, who determined that her cancer was slow growing, but resilient. He put her on several different drug regimens, but her cancer kept resurfacing.
“Generally, people who relapse after initial chemotherapy have a very poor prognosis,” Tuscano said. “It’s usually an indicator of a very resistant disease.”
In 2008 Tuscano enrolled her in a clinical trial combining rituximab, with Revlimid. The hope was that the immunomodulatory activity of Revlimid would combine with the B-cell antibody activity of the rituximab to more effectively fight the cancer. Mooney was one of the first in the world to have the combination therapy.
Mooney experienced a dramatic remission.
Eight years and more than 100 cycles of treatment later, there is no evidence of disease. Although declared cancer-free, Mooney has elected to stay on her therapy as an insurance policy against recurrence. Now that she doesn’t have to worry about cancer, Mooney spends most of her time babysitting her great grandchildren.
“I would never have dreamed of it,” Mooney said. “Let me tell you, it is a blessing.”
UC Davis scientists awarded $1 million grant for prostate cancer research
The Prostate Cancer Foundation and Movember, the movement that has raised hundreds of millions of dollars for men’s health research and programs and best known for encouraging mustache growth in November, have delivered $1 million to UC Davis prostate cancer researchers.

The funding will allow UC Davis basic scientist Hongwu Chen of the Department of Biochemistry and Molecular Medicine and his colleagues to further develop a novel approach to overcome treatment-resistant prostate cancer.
The project builds on the researchers’ recent finding that a receptor protein called RORgamma can be an important prostate cancer driver, and that small molecules targeting the ROR protein can effectively block tumor growth and circumvent drug resistance in pre-clinical models such as cell lines and in human tumors in mice.
Synthesis | UC Davis Comprehensive Cancer Center 
2279 45th Street | Sacramento, CA 95817 | Info: 916-734-5959 | Referrals: 916-703-5210
© 2015 UC Regents. All Rights Reserved | Legal | Jobs | About Us | News | Locate a Staff Member
