Innovative breast CT technology, developed at UC Davis, may out-perform
mammography and improve breast cancer survival odds
Just before Christmas last year, Cathryn Sant, a Gold River real estate broker, got the news many women fear. A routine screening mammogram had turned up a suspicious change in her left breast. A second scan confirmed the abnormality, and Sant's doctor recommended a needle biopsy.
"First, though, Karen Lindfors, the UC Davis radiology professor who read Sant's, invited her to participate in a research study of a new breast imaging , breast CT. Developed by UC Davis radiology professor John Boone with $6 million in grants from the National Institutes of Health and California Breast Cancer Research Program, the device recently reached clinical testing. Sant agreed.
When she arrived at the UC Davis Imaging Research Center for her breast CT, Sant was asked to lie face down on the experimental machine's padded table, so that first one breast, then the other, projected through a circular opening in. the table surface. As Sant held her breath, a CT scanner beneath the table rotated around each breast, taking about 17 seconds per breast. No breast compression was required.
Afterward, Sant had a needle biopsy. Cells removed from the suspicious areas seen on the mammograms were examined by a pathologist. The pathologist identified two early cancers, a ductal carcinoma in situ and a lobular cancer.
Radiologist Lindfors then compared Sant's mammograms with the images obtained by breast CT. Lindfors found that both technologies had picked up Sant's cancer; the investigational breast CT did as well as mammography.
Sant counts herself lucky that her cancer was found early, and is glad to have contributed to research that may lead to a new breast-cancer screening alternative.
She also has her own conclusions about the two technologies:
"If I had a choice, I'd choose the CT," she said. "It's a lot more comfortable.".
Traditional mammography remains the gold standard for the early detection of breast cancer. But mammography has its limitations, including reduced sensitivity in women with dense breasts or in women, like Sant, who have breast implants. Sant, now 57, had breast augmentation surgery at age 40.
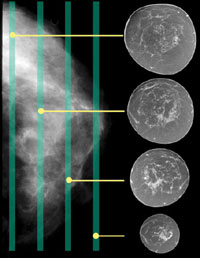
Because mammograms are X-rays taken through all the layers of the breast at once, they may miss a tumor hidden by other structures within the breast. The breast CT scanner, in contrast, rotates around the breast, acquiring a vast amount of raw image data that is then assembled by computer into about 300 highly detailed, threedimensional pictures of the breast.
"It's the difference between taking a picture of a crowd from across the street, versus circling the crowd and shooting hundreds of separate photos along the way, each photo only two or three people deep," said Boone, the machine's developer. "Your chances of finding a particular person in the crowd are going to be a lot better with more photos."
Sant was among the first volunteers in the Phase II clinical trial of breast CT at UC Davis. The trial, which will enroll about 190 patients in all, is open only to UC Davis patients with recent mammograms that are suspicious for breast cancer, and who will be undergoing needle biopsy to confirm the presence of cancer. Boone and Lindfors are the principal investigators.
If the trial confirms that breast CT detects tumors as accurately as mammography, as it did in Sant's case, the next step will be a larger, Phase III study to test whether Boone's machine can do more — detect tumors earlier than mammography. If all goes well, that trial could be under way within three to five years.
Detecting smaller tumors
"We think this technology may allow radiologists to routinely detect breast tumors at about the size of a small pea," Boone said. "In contrast, mammography detects tumors that are about the size of a garbanzo bean. Tumor size at detection is one of the most important factors in determining breast cancer prognosis, so if we can detect smaller cancers and do so routinely, survival from this disease will improve."
Computed tomography is used every day to scan brains, lungs, abdomens and pelvises. But imaging experts long ago dismissed CT as impractical for breast cancer screening, assuming it would require too much radiation. Boone decided to revisit the issue, recognizing that radiation-dose estimates for breast CT were based on use of standard CT machines, which would require the breast and entire chest to be scanned together.
A medical physicist who holds six scientific patents, Boone has been a consultant to the National Institutes of Health, U.S. Food and Drug Administration and U.S. Army Breast Cancer Research Program. He is vice chair for research in the UC Davis Department of Radiology and co-leader of the UC Davis Cancer Center's Biomedical Technology Program.
When he recalculated radiation doses based on scanning the breast alone, he found that CT imaging would use no more radiation than mammography.
The next step was to build a breast-only CT machine. Boone custom-designed a system consisting of a padded table over a floor-mounted CT scanner. His collaborators included Lindfors and J. Anthony Seibert, also a radiology professor at UC Davis, and Thomas R. Nelson, a radiology professor at UC San Diego.
Scientists at the University of Rochester, University of Massachusetts and Duke University have also been developing breast CT prototypes, but Boone's reached clinical testing first.
Breast PET-CT
In recent months, Boone and UC Davis PET physicist Ramsey Badawi have started work on another innovative machine, a breast PET-CT hybrid. Full-body PET-CT has been widely available for about four years, and has become an important tool in oncology for diagnosing and staging cancers and monitoring response to treatment (see Molecular Imaging).
Boone and Badawi are engineering a PET system that will clamp onto the breast CT machine and image just the breast. The machine would combine the fine anatomical detail provided by breast CT with the functional information derived from positron emission tomography detection.
For Sant, life is getting back to normal following a double mastectomy — her right breast also had abnormalities — and seven weeks of radiation therapy. She is enjoying her three grandchildren, ages 2 to 4, and is grateful for her excellent prognosis.
"The doctors were able to see everything they needed to see," she said. "And I'm here to talk about it."