Teaching an old therapy
new tricks
Melanoma, the most aggressive skin cancer, is also one of the most difficult to treat.
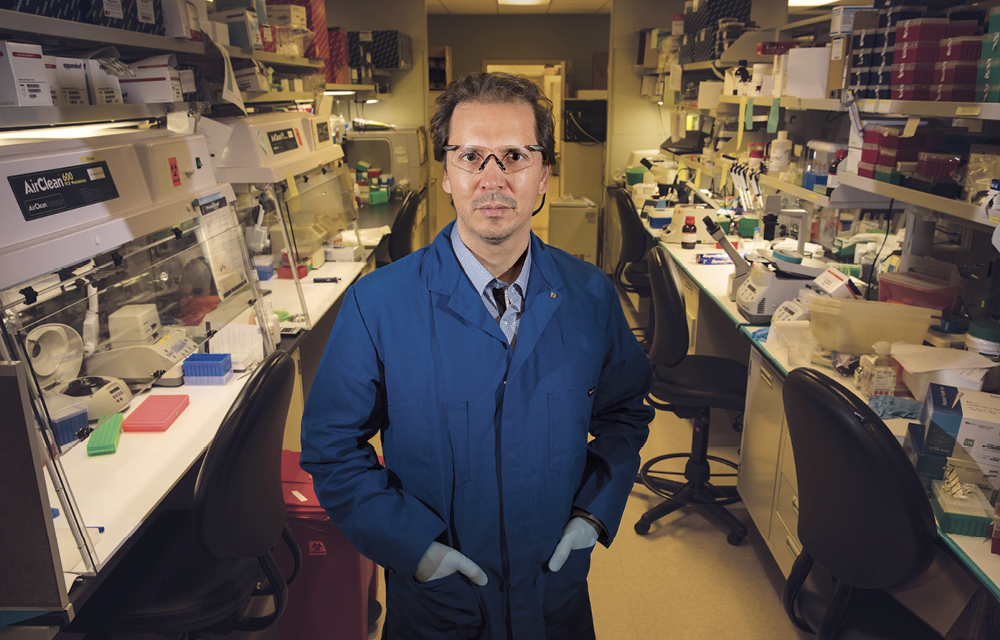
But Emanual Maverakis, associate professor in the UC Davis Department of Medical Microbiology and Immunology, has helped develop a new approach with an old therapy: interleukin-2 (IL-2). Instead of giving IL-2 systemically, where it can cause widespread side effects, Maverakis and colleagues are injecting it directly into surface lesions. The team hopes they can popularize this unique approach and help patients with metastatic melanoma around the world.
One of those patients is 75-year-old Larry Moberg, a retiree and avid tennis player from Sonora. Diagnosed with melanoma in April 2016, Moberg had surgery to remove the lesion and an affected lymph node. For several months, the cancer appeared to be gone, but late that summer it reappeared in the form of more than 20 small nodules on his arm. The surgeon sent him to see Maverakis.
But the side effects
IL-2 is a signaling molecule that can boost a patient’s immune response. When it worked, systemic IL-2 essentially painted a target on tumors so T-cells could attack. But it didn’t work often, and the side effects were horrific: fever, vomiting, diarrhea, rashes, liver issues, accelerated heart rate. Because melanoma typically does not respond well to chemotherapy, IL-2 became a fallback therapy.
“Systemic IL-2 works in around 9 percent of patients,” says Maverakis, “but a few years ago, we didn’t have any other treatment options. If you had 200 patients, maybe five of them could tolerate the full cycle with all the side effects. Even if they got the top-of-the-line therapy, the outcomes were dismal.”
But studies were coming from Europe that showed IL-2 could be injected directly into skin lesions rather than infusing it throughout the body. Maverakis was intrigued: intralesional injections could bring the medicine directly to the problem and significantly reduce side effects.
“I had patients with metastatic melanoma, and we decided to treat them using this European protocol,” says Maverakis. “I could see the tumors there, I thought we could just target the medication right to the melanoma, so it made a lot of sense to use it intralesionally.”
A hard sell
Despite the promising results in Europe and the fact that he was using lower doses of IL-2 in a more targeted fashion, not everyone was excited about the idea. With all the side effects, IL-2 had a nasty reputation. But the need was great, and cancer surgeon Steve Martinez, formerly with UC Davis, strongly encouraged Maverakis to move forward.
“The patients we were treating could never tolerate systemic IL-2,” says Maverakis. “IL-2 was already approved for melanoma. We were just administering it in a way that was less toxic.”
Maverakis and colleagues moved forward, and the therapy showed dramatic results. Not only did the 11 patients in the trial have a 100 percent response rate, but the side effects were minimal. Armed with these positive findings, Maverakis has incorporated intralesional IL-2 into his regular practice.
Moberg was an excellent candidate for the therapy and came in for six appointments, receiving four to six injections each time. As with the research trial, the regimen included an immune booster called imiquimod and topical retinoids, a form of vitamin A.
“The lesions are all gone,” says Moberg, “and as of this date, everything is fine. It did exactly what he said it would do.” As for side effects, Moberg experienced a mild chill a few hours after the injections, but that was it. And he’s back to his full tennis schedule.
Maverakis is obviously pleased with these results, but IL-2 still has a stigma, making many physicians reluctant to use it. However, the National Comprehensive Cancer Network recently incorporated the treatment into its guidelines, a move based, in part, on Maverakis’ published findings on the approach. Maverakis is reaching out to other cancer centers to help them replicate his results, and wants them to know that intralesional IL-2 and systemic IL-2 are two different animals.
“There are very few side effects,” says Maverakis. “We routinely treat patients in their 80s and 90s. We can treat cancers we couldn’t touch before.”
