Teaming up against childhood leukemia

"The whole world turned upside down at that point," says Terri Avilla, JP’s mother. "He would have been a freshman, but that all went to the wayside."
Five months into chemotherapy treatment, JP’s 230-pound frame had dwindled to 180 pounds. The drugs, aimed at killing the leukemia cells, also made him sick. An allergy to one of the agents gave him hives from head to toe and weakened his immune system. Many children treated with chemotherapy for leukemia suffer similar side effects.
"There are also lots of long-term effects," says Noriko Satake, who specializes in pediatric hematology and oncology at the UC Davis Comprehensive Cancer Center. "Chemotherapy and radiation therapy can harm bones, the heart and brain function. They affect a child’s growth and development."
Satake and two other UC Davis scientists are collaborating to find alternative, less toxic treatments for childhood leukemia. Satake and stem cell researchers Elva Diaz and Paul Knoepfler are studying the mechanisms of genes involved in leukemia and other types of childhood cancer, hoping that a better understanding of the molecular underpinnings of the disease will yield novel treatments, improve patient outcomes and reduce side effects. The multi-disciplinary, translational approach is designed to get targeted therapies out of the laboratory and to individual patients in the clinic when they need them.
Leukemia accounts for one-third of all childhood cancers, and ALL is the most common type of childhood leukemia. Robust, sweeping pediatric clinical trials have yielded dramatic results, bringing the overall leukemia survival rate to 80 percent. Still, Satake says, many children have poor outcomes because some leukemias resist treatment.
Leukemia accounts for one-third of all childhood cancers, and ALL is the most common type of childhood leukemia. Robust, sweeping pediatric clinical trials have yielded dramatic results, bringing the overall leukemia survival rate to 80 percent. Still, Satake says, many children have poor outcomes because some leukemias resist treatment.
"We know the bad cancer is out there," says Satake. "We are bringing the problem into the laboratory, creating a new treatment that is better than the current one and bringing the solution back to the patient."
Satake is working to develop a unique method to deliver a type of molecule called siRNA, along with nanoparticles and a linker, which interferes with gene expression and recognizes and binds to the surface of leukemia stem cells. Unlike normal cells, stem cells can make copies of themselves or become different kinds of cells.
"The linker is the key to preventing negative side effects in patients because the new treatments we are developing would target leukemia stem cells and not go into normal cells," says Satake.
Satake’s fellow researchers are focused on cancer genes Mxd3 and N-Myc.
"Both can be great targets in children’s cancer, but we don’t know the roles of each," says Satake. "What we learn about them will help us to find other targets and learn how cancer cells grow."

"If we can target cancer stem cells that have a lot of N-Myc, we can stop the cancer."
Diaz, an associate professor in pharmacology, studies the mechanisms behind Mxd3, and Knoepfler, an associate professor in cell biology and human anatomy at the UC Davis School of Medicine, researches N-Myc, both of which are found in high levels in cancer cells.
Knoepfler is studying the role that high levels of N-Myc havein uncontrolled cell growth. He explains that in cancer stem cells N-Myc acts as an accelerator, telling the cancer to grow unchecked into a full-sized tumor. In normal stem cells, however, N-Myc acts as the accelerator and other molecules as the brakes. In a healthy brain, for example, N-Myc tells the cells to grow during development and then turns off growth when the young adult brain reaches the correct size. In brain cancer stem cells N-Myc can turn cell growth back on, resulting in a cancerous tumor.
"My theory was that if we could understand the normal function of N-Myc in cells, that would help us understand how it causes cancer," says Knoepfler. "If we can target cancer stem cells that have a lot of N-Myc, we can stop the cancer."

"The goal of the collaboration with Noriko Satake is to develop novel therapies using Mxd3 as a target to treat childhood cancers such as leukemia."
Diaz focuses on Mxd3, a gene that regulates cell proliferation and is found both in normal stem cells and leukemia stem cells. Diaz hopes to understand the gene’s role in leukemia and whether it is a useful target for treatment. Because Mxd3 and N-Myc are in the same pathway, the two proteins likely share similar functions. Working together, the researchers aim to learn how N-Myc and Mxd3 interact to regulate cancer cell development and proliferation.
"The goal of the collaboration with Noriko Satake is to develop novel therapies using Mxd3 as a target to treat childhood cancers such as leukemia," says Diaz.
"The more targets we have, the better chance we have of killing the cancer cells," Satake adds. "If our approach is successful, the way we treat cancer in the future will be completely different from current treatments."
Satake eventually will conduct human clinical trials of any new treatment developed in the laboratory.
 Even JP has contributed to the research effort, having donated his own leukemia stem cells to Satake after his diagnosis. And while JP may not benefit directly from the research trio’s current work, he and his family are hopeful that his participation will aid in their efforts.
Even JP has contributed to the research effort, having donated his own leukemia stem cells to Satake after his diagnosis. And while JP may not benefit directly from the research trio’s current work, he and his family are hopeful that his participation will aid in their efforts.
Even JP has contributed to the research effort, having donated his own leukemia stem cells to Satake after his diagnosis. And while JP may not benefit directly from the research trio’s current work, he and his family are hopeful that his participation will aid in their efforts.
"The more information researchers have, the higher the survival rate for these kids," says Terri Avilla.
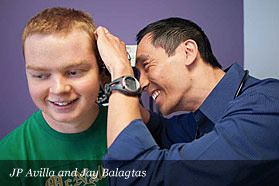
Today, JP is a husky 17-year-old high school student who earns excellent grades, has a part-time job at a local fast-food restaurant and enjoys Lake Tahoe vacations with his family.
"For missing 72 days of school he is still getting a 3.0, and that’s pretty darn good," says Terri Avilla of her son. "He is quick-witted and has always turned things around by joking with us or the nurses — even at his worst."







