Bits & pieces
Review by UC Davis researchers contributes to new prostate cancer screening recommendations
An exhaustive review by UC Davis researchers of more than 60 studies is the basis for new national prostate cancer screening recommendations. The U.S. Preventive Services Task Force recommends that for men ages 55–69 the decision to undergo periodic prostate-specific antigen (PSA)-based screening for prostate cancer should be an individual one and should include a discussion between the patient and his clinician about the potential benefits and harms of screening.
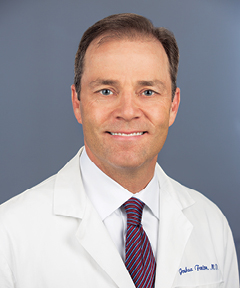
The task force determined that while screening offers a “small potential benefit of reducing the chance of death from prostate cancer in some men,” many men “will experience potential harms of screening.” Those include false-positive results that require additional testing and possible biopsy, over-diagnosis and overtreatment, and treatment complications such as incontinence and erectile dysfunction.
The new recommendation updates a prior one published in 2012, in which the task force concluded that screening benefits do not outweigh the expected harms enough to recommend routine screening.
The evidence was compiled and analyzed for the task force by a team at the UC Davis Center for Healthcare Policy and Research, and led by Joshua Fenton, a family medicine physician who has conducted numerous studies on the effectiveness of various cancer screening methods and technologies.
A 17-year legacy: AANCART tackled Asian American cancer health disparities
In 2000, the National Cancer Institute funded the Asian American Network for Cancer Awareness, Research and Training (AANCART) to reduce health disparities among Asian Americans. Headquartered at UC Davis Comprehensive Cancer Center since 2002, the group’s researchers poured their energy into investigating the unique cancer burden affecting Asian Americans. The grant ended in December 2017.
Asian Americans are the first U.S. population to experience cancer as the leading cause of death, and their cancers are disproportionately due to infectious agents such as viruses that cause liver cancer. High rates of tobacco use and lower rates of cancer screenings are additional challenges facing these populations.
To focus on this burden, AANCART developed linguistically appropriate materials in at least six Asian languages, cultivated culturally competent and trusting relationships with the community, trained bilingual/bicultural lay health educators, completed 12 randomized controlled studies and nurtured an impressive array of next-generation researchers.
Seventeen years and 218 published peer-reviewed papers later, AANCART achieved major milestones — some even unpredicted — in demonstrating that cancer risk behaviors can be significantly reduced for colorectal cancer and liver cancer among Asian Americans.
Other notable achievements included:
- Mentorship of new and early-stage investigators, many of whom pursued post-secondary degrees, published research as primary investigators and received awards, including Elisa Tong, winner of the UC Davis Dean’s Team Science Award; Shin-Ping Tu, the new chair of the Division of General Internal Medicine; and Julie Dang, director of the Cancer Center’s Community Engagement and Outreach;
- Creation of a bilingual (English/Spanish) video about advantages for HIV-positive patients to participate in cancer clinical trials, now in use in Puerto Rico;
- Collection and utilization of a record number of biospecimens to characterize cancer risk in Asian Americans; and
- Laying the foundation for a three-year Bristol-Meyers Squibb Foundation grant to increase cancer detection, care and prevention into primary care offered through Health And Life Organization (HALO), which runs community clinics in Sacramento.
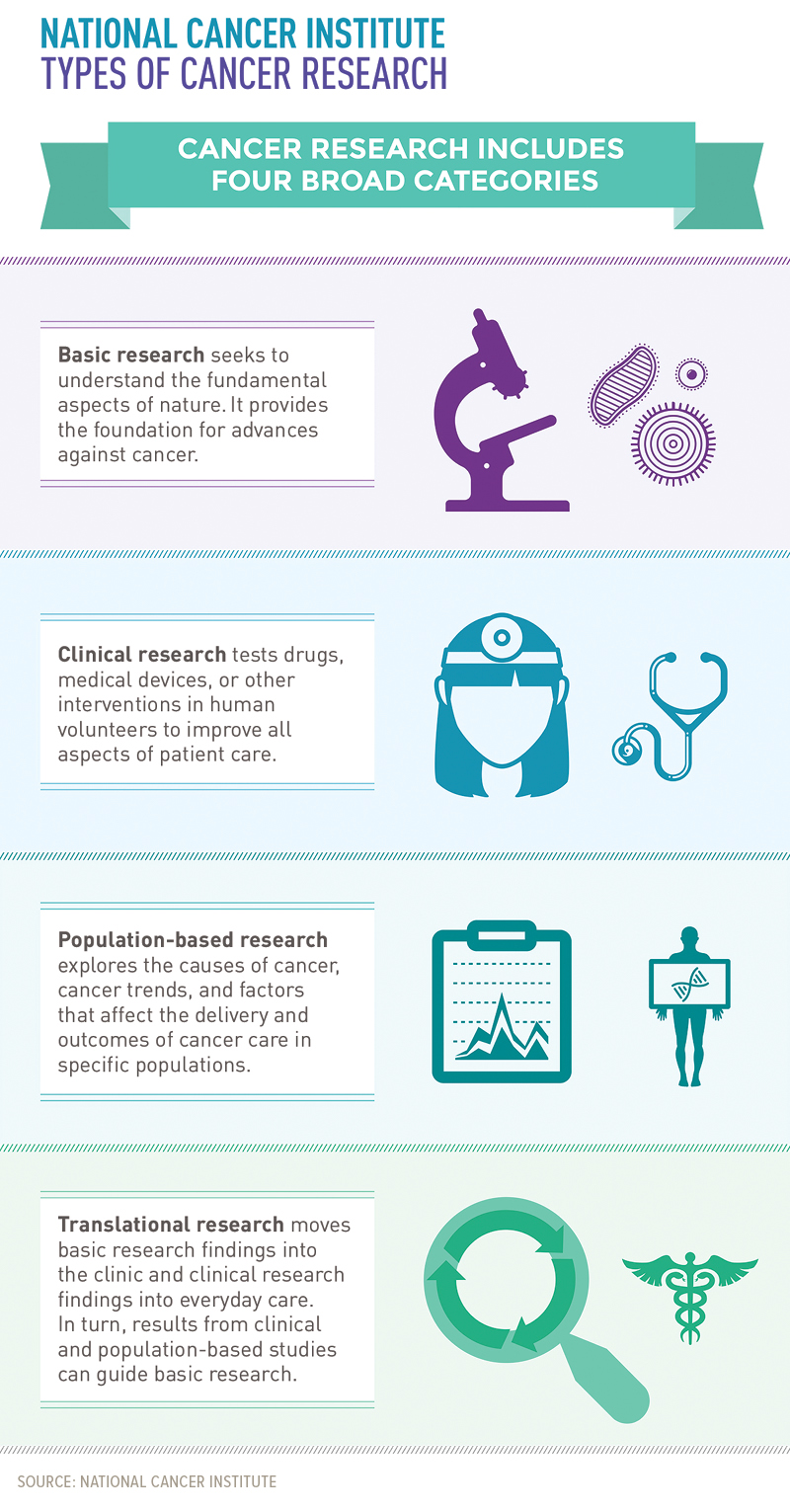
National Cancer Institute; Types of cancer research
Cancer research includes four broad categories:
Basic research seeks to understand the fundamental aspects of nature. It provides the foundation for advances against cancer.
Clinical research tests drugs, medical devices, or other interventions in human volunteers to improve all aspects of patient care.
Population-based research explores the causes of cancer, cancer trends, and factors that affect the delivery and outcomes of cancer care in specific populations.
Translational research moves basic research findings into the clinic and clinical research findings into everyday care. In turn, results from clinical and population-based studies can guide basic research.
Cancer Center and HALO collaborate to reduce cancer burden in Asian Americans
A collaboration spearheaded by UC Davis cancer specialists was launched June 1 to enhance cancer prevention and oncology care for up to 10,000 Asian Americans, Native Hawaiians and Pacific Islanders in Sacramento.
The UC Davis Division of Hematology and Oncology and Comprehensive Cancer Center are partnering with Health And Life Organization (HALO) and its community clinics to identify those at risk and get them the expert care they need.
The collaborative is led by Moon Chen, Jr., associate director for cancer control and cancer health disparities at the Cancer Center, and funded with a $750,000 grant from Bristol-Myers Squibb Foundation with additional support from the UC Davis Office of Research, Cancer Center and Clinical and Translational Science Center.
Cancer is the leading cause of death in Asian Americans, many of which are preventable. The collaborative will focus on interventions, including tobacco cessation and human papilloma virus vaccination, and screenings for cervical, liver, breast and colorectal cancers.
Screenings will take place at HALO clinics with support from bilingual health educators and UC Davis specialists who can help the clinics use the electronic medical record as a tool to alert providers about needed screenings and care.
Celebrating cancer survivors 2018: National cancer survivor day 2018; a celebration of life