Bits & pieces
Experimental compound may help prevent cancer progression
A study in mice of an anti-inflammatory compound developed in the lab of Cancer Center member Bruce Hammock has found that it suppresses inflammation that can occur from cell debris after cancer treatment and stimulate further cancer growth and recurrence.
“We are excited about this research and its potential,” said Hammock, a distinguished professor in the UC Davis Department of Entomology and Nematology. “Chemotherapy and surgery, the mainstays of conventional cancer treatment, can act as double-edged swords.”
The research by a 13-member team, including from Harvard Medical School, was published in the Proceedings of the National Academy of Sciences (PNAS).
The team treated mouse models of ovarian cancer with a dual lipid pathway inhibitor discovered several years ago in the Hammock lab. It integrates two anti-inflammatory drugs (COX-2 inhibitor and soluble expoxide hydrolase (sEH) inhibitor) into a single molecule with the aim of reducing tumor angiogenesis and metastasis.
“The dual inhibitor here follows earlier work we did with it, blocking breast and lung tumors in mice,” Hammock said. “It is already being clinically evaluated for its therapeutic properties in other diseases.”
Lead researcher Dipak Panigrahy, a former Harvard physician turned full-time researcher, described chemotherapy and surgery “as our best tools for front-line cancer therapy, but chemotherapy and surgery create cell debris that can stimulate inflammation, angiogenesis and metastasis. Thus, the very treatment used by oncologists to try to cure cancer is also helping it survive and grow. Overcoming the dilemma of debris-induced tumor progression is critical if we are to prevent tumor recurrence of treatment-resistance tumors which lead to cancer therapy failure.”
The tumor cell debris generates a “cytokine surge” that can result in a perfect storm for cancer progression, and the dual inhibitor acts as a surge protector,” Panigrahy said. “Our studies potentially pave the path for a new strategy for the prevention and treatment of chemotherapy-induced resistance with potential to translate to the clinic. If successful, this approach may also allow us to reduce the toxic activity of current treatment regimens.”
American Cancer Society statistics show that among women, ovarian cancer ranks fifth in cancer deaths. A woman’s risk of ovarian cancer is about 1 in 78; every year more than 14,000 die from the disease.
“We are exploring all options to translate this compound to cancer patients especially in combination with current cancer therapies such as chemotherapy, radiation, immunotherapy, or surgery which either directly or indirectly may generate tumor cell debris,” Panigrahy added. “Our next step is to investigate whether our findings are consistent with clinical studies involving human cancer.”
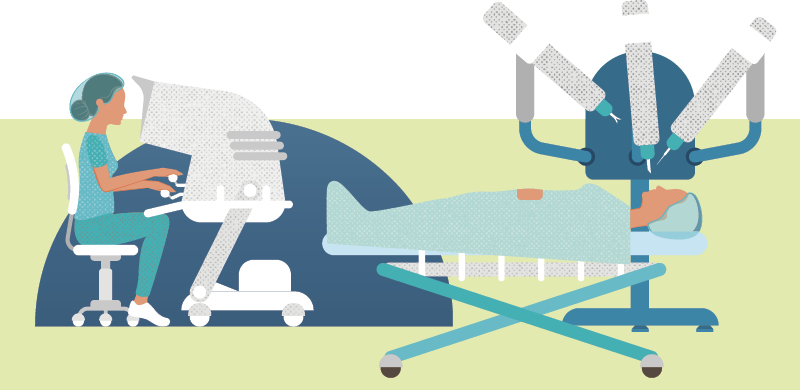
Optical device aids robot-assisted cancer surgery
For hard-to-reach tumors at the back of the throat, robots can assist surgeons to remove cancers in a less invasive way. But this high-tech approach has a drawback: the surgeon’s inability to assess through touch whether they’ve been able to get all of the cancer.
An innovative new device developed by UC Davis biomedical engineer Laura Marcu is helping to change that. Based on fluorescence lifetime imaging microscopy (FLIm), the device can be used in tandem with robotic surgery to distinguish between cancerous and benign tissue, guiding the physician in real time to achieve a more precise surgical outcome for the patient.
In a first-in-human, proof-of-principle study published in Scientific Reports, a Nature publication, UC Davis researchers reported on their ability to successfully integrate the FLIm tool with a surgical robot to allow real-time evaluation of the different tissue types in patients undergoing oral cancer surgery without using contrast agents. First studied in animal models, the technology has now been used in about 30 human patients with cancers of the tonsil and base of the tongue.
“We are the first to demonstrate implementation of augmented reality in patients and in conjunction with robotic surgery,” said Marcu, a professor and Cancer Center member.
FLIm measures the autofluorescence properties of certain molecules in tissue in the form of wavelength (or color) and lifetime (or the time a molecule emits light). Since tumor tissue is made up of molecules different from those in normal tissue, tumors also have different fluorescence properties. This allows the autofluorescence to encode diagnostic information to help the surgeon as he removes tissue.
“The FLIm features are augmented instantaneously in the surgeon’s field of view so the surgeon can see tissue properties that cannot be seen otherwise,” Marcu said.
Marcu teamed up with Cancer Center member D. Gregory Farwell, professor and chair of the UC Davis Department of Otolaryngology — Head and Neck Surgery, to use the device to help guide him during complex oral cancer surgeries. When Farwell began using the robot to do complex head and neck surgeries, the two figured out a way to incorporate the device with the robot’s technology.
“These tumors are very difficult to access, and they traditionally required extensive surgery that involved cutting the jaw and reconstructing the jaw to allow us to get back there,” Farwell said. “In selected patients we can use the robot to gain access to tumors that historically we could not get to less invasively.”
FLIm uses light to excite molecules in tissue and measure how long they emit light of their own after they are excited. Different types of molecules emit light at different rates. FLIm can measure the rates, and that information is used to distinguish between different types of tissue. The device employs fiber optics to deliver and collect the light. Marcu and Farwell are recruiting up to 80 more patients to further develop and refine the technique. Marcu also plans to team with urological surgeons to use the device for prostate cancer patients.
UC Davis team takes on pancreatic cancer with SU2C grant
UC Davis scientist Julie Sutcliffe and surgical oncologist Richard Bold have been awarded a $1 million “New Therapies Challenge” grant from the Pancreatic Cancer Collective in an effort to improve survival for people with the disease.
The Collective is a strategic partnership of the Lustgarten Foundation and Stand Up To Cancer (SU2C). The UC Davis team was one of seven to receive the grant, which could be augmented by an additional $4 million in the second round of funding.
The UC Davis team will use the grant to build on nearly 15 years of work undertaken in Sutcliffe’s laboratory, which developed advanced imaging techniques to pinpoint pancreatic cancer using positron emission tomography with a specially synthesized peptide that binds to tumor cell receptors. The team will now develop the radiotherapy that can be delivered through a radioactive isotope using the same peptide. The radiotherapy will attack a protein called integrin αvβ6, which is significantly upregulated in pancreatic cancer and is a marker for cancer aggression.
“We have an opportunity through this funding to take our diagnostic agent and turn it into a therapy,” said Sutcliffe, professor in the Departments of Internal Medicine and Biomedical Engineering. “Over the next few months we will design and synthesize the targeted therapy, test its efficacy in animal models and prepare for translation to the clinic by the end of the 14-month proposal.”
Sutcliffe noted that similar radiotherapies have been developed and are in clinical trials for treatment of prostate cancer, neuroendocrine pancreatic cancer and other neuroendocrine tumors.
“There is a clear need right now for more effective pancreatic cancer treatment,” said Bold. “There is very little out there and the 5-year survival rate is not improving.”
At year’s end the UC Davis team will report their results to the Collective, and teams deemed to have the most promising treatment approaches will advance to the second round and receive $4 million to support clinical trials.
Sutcliffe said she is proud and thrilled to be part of the international SU2C effort.
“It is a great honor to receive this prestigious grant and the opportunity to improve outcomes for people diagnosed with pancreatic cancer,” she said. “Working in tandem with other leading clinicians and scientists around the country and beyond, I believe we can make the difference so desperately needed.”
Kit Lam becomes the Sue Jane Leung Presidential Chair in Cancer Research
Kit Lam, chair of the UC Davis Department of Biochemistry and Molecular Medicine, is the inaugural holder of the Sue Jane Leung Presidential Chair in Cancer Research.

The presidential chair is the result of a $1.5 million gift to UC Davis from the family of Sue Jane Leung and a $500,000 contribution from the UC Office of the President. Lam also serves as co-director of the UC Davis Comprehensive Cancer Center’s Cancer Therapeutics Program.
Sue Jane Leung, who never smoked, was diagnosed with lung cancer in 2006 and fought the disease with tenacity until her death five years later. Her daughter, Lucinda Hsu, and her husband, James Leung, a UC Davis engineering graduate, decided to make the gift to UC Davis to honor Sue Jane’s strength and determination.
Lam, who has pioneered novel approaches to cancer drug delivery, said the generous gift from the Leung family will allow the Cancer Center and Department of Biochemistry and Molecular Medicine to build a world-class cancer drug development and drug delivery program.
“The Department of Biochemistry and Molecular Medicine and I are very grateful for the Leung family’s generosity, and their foresight in supporting research in the development of novel cancer therapy,” Lam said.

