New bioengineered scaffold may help large deep burn wounds heal faster
Study shows supportive structure may reduce risk of complications and need for grafting
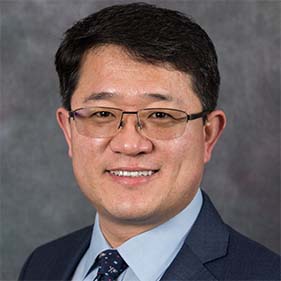
A team of UC Davis researchers led by bioengineer Aijun Wang has designed and tested a supportive structure, called a scaffold, that can help large deep burn wounds heal faster. The promising new treatment was found to promote the formation of new blood vessels and reduce complications linked to open burn wounds. It may also reduce the need for skin grafting in patients with significant burns over their body.
Scaffolds are made of an engineered biomaterial that provides support for new tissue formation. Normal skin tissue contains skin cells and an extracellular matrix that harbors proteins and small molecules that help repair and nourish tissue. These cells and extracellular matrix elements are lost at large deep burn wound sites.
Wang and his team engineered a scaffold that is modified with a special molecule known as LXW7 that specifically interacts with endothelial cells to help the wounds heal.
“Endothelial cells play a critical role in the body’s homeostasis and regeneration. They help in blood vessel formation during wound healing and regulate the movement of substances across the body,” said Wang, professor of surgery and biomedical engineering. He is also the vice chair for translational research, innovation and entrepreneurship in the Department of Surgery and co-directs the Center for Surgical Bioengineering at UC Davis, and leads the Wang Lab.
“At UC Davis, we developed the LXW7 molecule that can specifically interact with endothelial cells and help in their attachment, migration and survival. Commonly used scaffolds lack specific binding sites to endothelial cells. When LXW7 molecules are added to scaffolds, they provide a gripping site for endothelial cells to bind, which allows for better interaction between the cells and their supportive structure known as extracellular matrix,” Wang explained.
Without a good blood supply and enough nutrients, the cells can’t regenerate, and the wound will take longer to heal.” —Aijun Wang, professor of surgery and biomedical engineering
In their study published in Frontiers in Pharmacology, the team showed that the engineered scaffold can accelerate wound healing in mice and lower the risk of burn complications, such as fluid losses and infection.
The study also indicated that the engineered new scaffold may reduce, or even remove, the need for autografting — the transplantation of the patient’s skin from one body part to the burn location. With the new scaffold, there is less risk of autografting complications, especially in patients with little skin that can be used for the procedure.
Risk of complications in deep burn wounds
Large deep burn wounds have a unique and complex healing process.
Deep burn injuries result in damaged blood vessels and skin tissue loss. Due to the large amounts of tissue loss, these wounds suffer from fluid and heat loss, higher infection rates, prolonged time for wound bed preparation before autografting, and an increased need for skin autografting. Such complications can result in painful scar formation and a higher risk of debilitating contractures, a skin tightening condition that affects the muscles, joints and tendon and requires long term physical therapy.
It is important to rebuild the blood vessel network in the wound bed. Blood vessels are critical to deliver oxygen and nutrients needed to allow cellular proliferation, migration and tissue regeneration. So, revascularization is key for tissue regeneration.
“Blood vessels are very important for generating new tissue. Without a good blood supply and enough nutrients, the cells can’t regenerate, and the wound will take longer to heal,” Wang said.
Testing the new scaffold for deep burn wound treatment
The research team wanted to find out what type of scaffold would best promote the formation of new blood vessels — a process known as angiogenesis. They used a commercially available collagen-based scaffold to test four different types of scaffolds on a large deep burn wound model in mice.
The biomaterial types are:
- collagen scaffold only
- collagen scaffold seeded with endothelial cells
- collagen scaffold modified with a combination molecule of a collagen-binding peptide bound to dermatan sulfate and LXW7
- collagen scaffold modified with the same combination molecule in conjunction with endothelial cells
The team applied the scaffolds on the deep skin burn wounds. They took photos for wound healing measurements on days 1, 7, 14, 21, 28 and 35 after treatment.
The wound healing process consists of four overlapping phases: homeostasis, inflammation, proliferation and remodeling. The study showed that the combined treatment loaded with endothelial cells had a higher wound healing rate in the proliferation phase. It accelerated key processes such as wound healing rate, re-epithelialization, vascularization and collagen deposition at Day 35.
“The combined treatment not only allowed the survival of the seeded endothelial cells, but also accelerated the recruitment of the body’s endothelial cells. It has the potential for treating large areas of deep burns by building a better-quality wound base and improving wound healing,” Wang said.
The leading authors on the study are Hengyue Song and Kewa Gao from UC Davis. Other coauthors include Dake Hao, Andrew Li, Ruiwu Liu, Bryan Anggito, Boyan Yin, Qianyu Jin, Vanessa Dartora, Kit S. Lam, Lucas R. Smith, Alyssa Panitch, and Diana L. Farmer from UC Davis, and Jianda Zhou from The Third Xiangya Hospital of Central South University, China. Song, Gao, Hao, Farmer and Wang are affiliated with Shriners Children’s Northern California.
This work was in part supported by the Shriners Hospitals for Children developmental research award (87200-NCA-19), Postdoctoral Research Fellowship (84704-NCA-19), the University of California Tobacco Related-Disease Research Program (TRDRP) High Impact Pilot Award (T31IP1530), and the California Institute for Regenerative Medicine (CIRM) grant (TRAN3-13332).
Title of Article: Engineered multi-functional, pro-angiogenic collagen-based scaffolds loaded with endothelial cells promote large deep burn wound healing.
Related Stories:
UC Davis wins $3 million CIRM grant to develop smart vascular graft for kidney patients