California cancer patients now have greater access to life-saving biomarker testing
New law mandates insurance coverage for genetic testing of tumors, ensuring more effective treatment
The University of California helped enact a critically important new state law that takes effect this month. It ensures cancer patients get access to biomarker testing to ensure they are receiving the best treatment.
Biomarkers are genes, proteins and other substances that can help pinpoint the molecular drivers of cancerous tumors. Biomarker testing has become an essential part of “personalized medicine,” which tailors treatment depending on the biological makeup of tumors.
“Knowing the biology of cancer is essential to identifying the most effective treatments,” UC Davis Comprehensive Cancer Center Director Primo “Lucky” Lara Jr. said. “Biomarkers can help doctors better see what makes certain cancers tick, allowing for a more personalized approach to diagnosing and treating the disease.”
Knowing the biology of cancer is essential to identifying the most effective treatments.”—Primo “Lucky” Lara Jr., director, UC Davis Comprehensive Cancer Center
Opening access to genetic testing
Until this year, a lack of insurance coverage has often blocked patients from accessing biomarker testing. Authored by California State Senator Monique Limón, the new law prevents that by mandating Medi-Cal and private health plan insurers to cover medically necessary biomarker testing as of July 1.
The University of California joined the American Cancer Society Cancer Action Network to co-sponsor Senate Bill (SB) 496 in 2023. The University of California Cancer Consortium provided expert insights during the bill making process. Following the Legislature’s passage of the bill last year, Gov. Gavin Newsom signed it into law.
“Everyone should have equitable access to these life-saving tests regardless of their insurance provider. That’s why SB 496 is a win for all Californians with cancer,” Lara said.
Targeted cancer therapy

Not all cancer cells are alike. The American Cancer Society said that even people with the same type of cancer can have different gene changes or different levels of certain proteins that can help the cancer cells grow. Biomarker testing can be helpful because these changes might also affect how well the cancer responds to certain types of treatment, such as targeted drug therapy and immunotherapy.
Checking a person’s tumor cells for these changes helps ensure that patients receive the right treatment at the right time. Targeted therapies can be less toxic than standard chemotherapy while being more effective.
“Improving access to biomarker testing can not only achieve better outcomes, improve quality of life and reduce costs but it is also key to reducing health disparities,” Lara said.
UC Davis Hereditary Cancer Program
Genetic testing can help determine whether a mutation is the underlying cause of a patient’s cancer and whether they have a higher risk of developing additional cancers. Testing, through blood or saliva sampling, also helps inform family members of cancer patients about their potential risk of getting cancer due to an inherited predisposition to cancer.
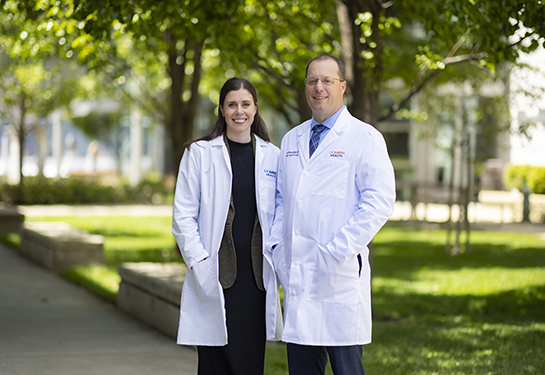
“If two or more of your relatives on the same side of the family have been diagnosed with breast, ovarian, uterine or colorectal cancer, it is wise to talk to a genetic counselor,” said Jeanna Welborn, director of the Hereditary Cancer Program at the cancer center.
Welborn and her team of licensed and certified genetic counselors and physicians provide cancer genetics services. These include cancer risk assessment, pre-test counseling, genetic testing, post-test counseling and personalized recommendations for cancer screening and risk reduction by practicing healthy habits.
“At some point, testing for an inherited predisposition to cancer may become routine,” Welborn said, although she stresses that patients should be comfortable with knowing the information.
“Many people who inherit a gene variant will never get cancer, so it is important that people don’t panic or live in fear,” Welborn said. “What’s key is knowing you may have a higher risk of certain types of cancer, which could help catch cancer earlier or prevent it altogether.”
Find out more about the Hereditary Cancer Program: 800 770-9261.
UC Davis Comprehensive Cancer Center
UC Davis Comprehensive Cancer Center is the only National Cancer Institute-designated center serving the Central Valley and inland Northern California, a region of more than 6 million people. Its specialists provide compassionate, comprehensive care for more than 100,000 adults and children every year and access to more than 200 active clinical trials at any given time. Its innovative research program engages more than 240 scientists at UC Davis who work collaboratively to advance discovery of new tools to diagnose and treat cancer. Patients have access to leading-edge care, including immunotherapy and other targeted treatments. Its Office of Community Outreach and Engagement addresses disparities in cancer outcomes across diverse populations, and the cancer center provides comprehensive education and workforce development programs for the next generation of clinicians and scientists. For more information, visit cancer.ucdavis.edu.