In early 2023, UC Davis Medical Center earned designations in Nurses Improving Care for Healthsystem Elders (NICHE) Senior Friendly and Age-Friendly Health Systems Committed to Care Excellence. Driving both efforts was Anna Satake, a Doctor of Philosophy (Ph.D.) graduate from the Betty Irene Moore School of Nursing at UC Davis.
The fact that her newly minted doctorate and industry-leading accomplishments happened in the same space of time are not a coincidence.
“I was open to new angles and ideas for me to take my career in older-adult care. I realized professionally that I was really frustrated with the system,” she says. “The School of Nursing taught me to scrutinize the literature and synthesize large data more clearly. A Ph.D. teaches you how to learn even better, makes you learn deeper.”
As a geriatric clinical nurse specialist (CNS), Satake says she always works to improve systems in order to improve outcomes. The older-adult population she chose to focus on in her career is a calling.
Geriatric focus gains momentum
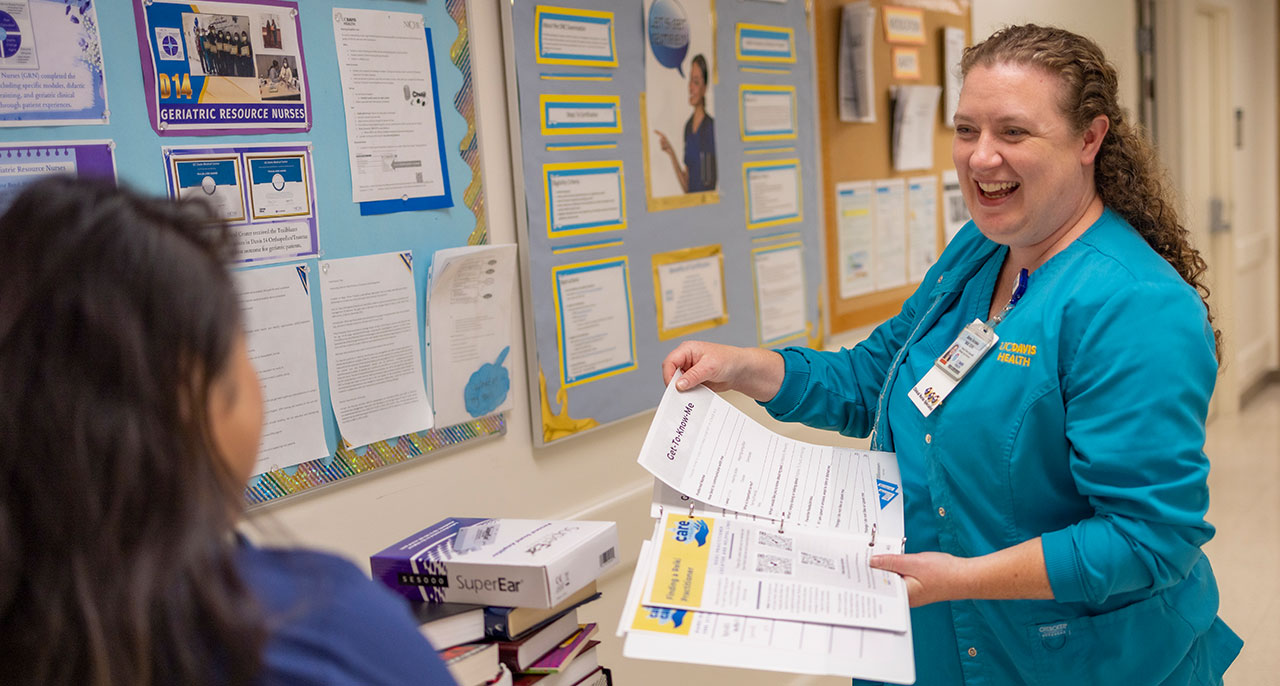
Satake led the Age-Friendly and NICHE designation efforts at the medical center. The education and geriatric resource nurse training program required by NICHE complemented the 4M implementation in day-to-day activities. What matters, mobility, medication and mentation (mental sharpness) make up the 4Ms.
“Clinical Nurse Specialists have clinical skills that enable them to develop and refine precise clinical workflows and educate the nurses who will undertake care improvements,” says Katren Tyler, vice chair for Geriatric Emergency Medicine and Wellness at UC Davis Health. “They are change agents for improving clinical workflows, and guide and educate the nursing workforce on improving the care of older adults.”
To focus on what matters to patients, floor nurses are encouraged to use the patient white boards to write specific daily goals. The geriatric resource nurses are trained on bedside assessments for older adults which help focus on high-risk geriatric syndromes to improve patient outcomes. Research shows that adapting protocols and implementing evidence-based practices improve health outcomes for older adults.
“What’s great is that UC Davis Health has dedicated the resources to have our geriatric nurses trained, so they can problem solve,” Satake says. “It has started a fire of engagement and they are initiating projects to implement change.”
Opening new doors
For two decades, Satake says she’s been trying to “find my tribe” in the hospitals in which she has worked. Fortunately, at UC Davis Health, she had supporters from the School of Nursing who advanced her work and elevated her profile.
“The relationships I formed with faculty brought advising and comfort. Their support showed we me have shared goals,” she says. “It also helped formulate a support system for me in UC Davis Health’s Healthy Aging Initiative.”
The initiative, launched in late 2019, leverages clinical care, research and education for age-friendly services that increase access to care, improve quality of life and make navigating the health system easier. Satake credits her clinical expertise, School of Nursing connections and Ph.D. degree to new doors being opened.
She collaborates on a project testing a clinically validated interactive behavior modification platform that distracts, engages and de-escalates anxious and/or aggressive behaviors associated with delirium in the ICU setting. She is also part of a group, led by Tyler, that’s developing a predictive model for incident delirium after admission to the hospital following presentation to the Emergency Department.
Her ultimate goal: expanding the commitment to geriatric care.
“It’s already opened doors with different leaders who want to help. It’s attractive to be around people with a passion for it,” she says. “Hopefully what that means is more resources assigned to look at more data to improve care. It’s an honor to care for people and advocate for people who can’t advocate for themselves.”