RESEARCH AND TECHNOLOGY — RADIATION ONCOLOGY
Research
The nationally recognized faculty in the UC Davis Department of Radiation Oncology focus their research on innovative treatment approaches to manage many cancers types.
Our broad interests include clinical trials and translational research on a variety of subjects. Some of our focus is on low-dose radiation biology, 3-D conformal radiation therapy, intensity-modulated radiotherapy, stereotactic radiotherapy and radiosurgery, high-dose radiotherapy, chemoprevention, quality of life, image-guided radiotherapy and translational research. Numerous departmental databases have been established that emphasize clinical outcomes and image-guided radiotherapy for performing high-quality, retrospective research. Our research has been published in many high-profile journals, and is frequently cited by radiation oncologists outside our facility.
Research Divisions
Advanced Treatment Technologies
We are at the forefront in providing the latest treatment technologies for cancer, using the highest quality equipment. The physicians, physicists and faculty at UC Davis Health are well-established experts in their field, and are recognized as experienced, national leaders in advanced technology and treatment. UC Davis Health is often one of the first facilities to offer the newest advances in the field, providing patients the best opportunities in their fight against cancer.
UC Davis Health offers the following advanced treatment options for cancer patients:
For more than a decade, UC Davis has been one of only a few hospitals in the Sacramento Valley to offer HDR brachytherapy and is a recognized leader in the field.
HDR brachytherapy is a state-of-the-art cancer treatment that places the radioactive source inside or in contact with the body — as opposed to treatment with an external beam. HDR brachytherapy can be used to treat several different types of cancer, including gynecological, breast, and prostate. High-dose, localized radiation is inserted temporarily, delivering the treatment quickly to the tumor and limiting the dose on adjacent body organs. HDR is often done on an outpatient basis, and can reduce treatment time from six to eight weeks of daily external radiation therapy to as little as three to 10 days, depending on the type of cancer being treated. If patients also need chemotherapy, HDR brachytherapy allows them to start that treatment sooner, possibly improving their chances for a cure. Compared to conventional treatments, HDR brachytherapy can result in fewer side effects as well. After treatment, the radiation source is removed from the patient and the patient is no longer radioactive.
HDR brachytherapy is highly effective for treatment of cervical cancer as an alternative to surgical removal of the cervix and uterus. It is also often used prevent recurrence of some cancers following surgery.
Our advanced HDR brachytherapy program uses the following treatments:
SAVI Breast Brachytherapy Device
SAVI is one of the newest technologies in accelerated partial-breast radiation therapy, and UC Davis is one of the few cancer centers in Northern California that offer this life-saving procedure.
SAVI is a breast brachytherapy device that has the unique ability to conform to the exact size and shape of each patient’s lumpectomy cavity — precisely controlling the radiation dose to the former site of the tumor. While similar to the more commonly used balloon catheter devices, SAVI offers significantly more precision and allows the radiation oncologist to tailor to each patient’s specific anatomy and disease process. It is also often more suitable for women of all breast sizes.
The SAVI applicator, which may be placed at the time of the lumpectomy or as a separate outpatient procedure, is a bundle of tiny, flexible catheters that can be opened as needed to fit the cavity. The radiation oncologist uses the catheters to apply the exact radiation dose needed for each portion of the breast, while at the same time protecting the surrounding healthy tissue such as the heart, lung, ribs and chest wall. In addition to the comprehensive safety measures that UC Davis maintains, the new SAVI device includes several built-in safety controls to ensure that each patient’s treatment is both safe and effective.
Due to the precise nature of the treatment, SAVI radiation treatment takes only five days, a significantly shorter amount of time than conventional treatment. Twice a day, the SAVI applicator is connected to the radiation source for about 5-10 minutes. Once the five-day treatment is completed, the SAVI device is removed by the radiation oncologist and the incision site simply needs to be cleaned and bandaged.
Gynecological HDR
UC Davis has a variety of sophisticated radiation implantation devices for gynecological brachytherapy treatment, including the state-of-the-art GammaMed HDR device. This treatment planning system accelerates therapy time, provides for more accurate treatment and produces fewer side effects. It also allows for dramatically better image processing, which aids the radiation oncologist in delivering the most precise and targeted doses possible.
All of the treatment machines used for gynecological HDR brachytherapy at UC Davis are capable of conforming to each patient’s particular anatomy and tumor specifications. They also offer top-notch safety features that limit exposure to nearby, critical tissues such as the vagina, bladder and rectum.
UC Davis offers the most innovative techniques in prostate brachytherapy, thanks to our expert radiation oncologists who have performed this sophisticated treatment for many years. Permanent prostate cancer brachytherapy, also called radioactive seed implant therapy, is an advanced technology that places radioactive seeds close to or directly in the tumor. Because the seeds are so close to the cancer cells, the cancer cells get inundated with radiation while the rectum, bladder, penis and other tissues receive minimal radiation. With seeds, a higher equivalent radiation dose may be delivered to the prostate than with traditional, external beam radiation.
Up to 125 tiny radioactive seeds about the size of a sesame seed are implanted into the prostate with guidance from ultrasound and X-rays. These seeds are so small that patients do not feel them. The radiation from the seeds kills the cancer cells over a period of a few months. How long the seeds remain radioactive depends on the radioactive material used and its dose. The seeds can safely remain in the prostate for the rest of a person’s life. The radioactive isotopes used are iodine or palladium.
Seed implant therapy is not new; the technique has actually been around for decades. However, recent advances in imaging technology have made it possible to view the prostate more effectively and place each seed more precisely.
Seed implant brachytherapy is considered minor surgery as it mostly uses local or regional anesthesia (although sometimes general anesthesia is used). It is usually a one-day, outpatient procedure, with little disruption of normal work or other activities and a short recovery time. Patients are recommended to avoid being close to children and pregnant women for a few weeks. Although the seeds continue to emit radiation for some time, most of the dose is absorbed by the surrounding tissue and very little penetrates the body.
In addition to seed implant therapy, there are also other options for patients with prostate cancer. Some patients may be candidates for the SpaceOAR, which allows patients to have an absorbable, injectable donut-like object inserted between the prostate and rectum. The SpaceOAR allows enough space to reduce the typical side effects from radiation treatment that occurs and protect more of the healthy tissues that may impact patients.
 Perfexion® Gamma Knife radiosurgery enables physicians to treat a wide variety and range of brain lesions — as well as some head and neck tumors — and offers shortened treatment times.
Perfexion® Gamma Knife radiosurgery enables physicians to treat a wide variety and range of brain lesions — as well as some head and neck tumors — and offers shortened treatment times.
This procedure focuses radiation directly at the tumor, preserving the surrounding, healthy tissue. The treatment is so precise that it if often called Gamma Knife “surgery,” but no surgical incisions are made. It is both non-invasive and painless and may even allow the option of frameless delivery through ICON, based on specific disease-site parameters. The Perfexion system is currently available in the Sacramento region only at UC Davis Comprehensive Cancer Center.
Our Perfexion robotic radiosurgical system provides precise tumor targeting, delivering a focused dose of radiation. It allows for simultaneous non-invasive treatment of multiple brain lesions — in one single automated procedure, in one single day — thus freeing patients from multiple radiation treatments and enabling them to quickly return to a normal routine.
The Gamma Knife system is proving to be ideal for areas that cannot be reached by surgery. Patients who cannot tolerate surgery or who have had previous radiation therapy to the brain may also be candidates for Gamma Knife.
Gamma Knife surgery is ideal for:
- Cancer that has metastasized (spread) to the brain, head or neck area
- Glioma/astrocytoma (malignant brain tumor)
- Acoustic neuromas/vestibular schwannoma (benign tumor on nerve leading to inner ear)
- Pituitary tumors
- Chordoma (benign tumor at base of the skull or lower spine)
- Craniopharyngioma (benign tumor at base of the skull)
- Hemangioblastoma (benign tumor of nervous system)
- Meningioma (benign tumor of protective membranes around brain and spinal cord)
The UC Davis Department of Radiation Oncology is among the first facilities to use this sophisticated, 3-D conformal radiation therapy and has been successfully providing treatment for many years.
Intensity modulated radiation therapy (IMRT) is an advanced, precise form of radiation therapy that delivers higher doses of radiation to the tumor and lower doses to nearby healthy tissue. IMRT allows patients to receive more concentrated radiation each day, potentially shortening the overall treatment time and improving treatment success. Some patients also experience fewer side effects during IMRT than more conventional treatment.
The radiation is delivered by a linear accelerator equipped with a multileaf collimator which helps to shape or sculpt the beams of radiation. The machine producing radiation can be rotated around the patient so that beams can be delivered from the best angles. Carefully planned and precisely manipulated beams conform as closely as possible to the shape of the tumor.
IMRT planning is done using sophisticated computer software that shapes the radiation dose to what the radiation oncologist specifies. Treatment is planned using 3-D computed tomography (CT) images of the patient in conjunction with computerized dose calculations to determine the dose intensity pattern that will best conform to the tumor shape. Instead of radiation coming out of the machine via a single beam, IMRT uses as many as 80-120 sliding metal leaves to shape the beam to fit the specific shape of the tumor or treatment site. The beam is actually composed of thousands of tiny beamlets. The metal leaves and manipulability of the beam prevent radiation from getting to nearby healthy tissue.
Although IMRT is primarily used to treat tumors in the brain, head and neck, nasopharynx, breast, liver, lung, prostate and uterus, this new technology is not always appropriate or necessary for every patient and/or type of cancer.
UC Davis provides three IMRT modalities, using Elekta Versa high-definition (HD) Blue and Gold linear accelerators and the helical TomoTherapy. For planning, the team employs the Raystation planning system.
 The UC Davis Department of Radiation Oncology was the first facility in the Sacramento Valley to utilize Image Guided Radiotherapy (IGRT) technology and, as a result, is a recognized, national leader in this technology. The department offers three linear accelerators capable of IGRT: Elekta Versa high-definition (HD) Blue and Gold machines and a Helical TomoTherapy HI-ART system.
The UC Davis Department of Radiation Oncology was the first facility in the Sacramento Valley to utilize Image Guided Radiotherapy (IGRT) technology and, as a result, is a recognized, national leader in this technology. The department offers three linear accelerators capable of IGRT: Elekta Versa high-definition (HD) Blue and Gold machines and a Helical TomoTherapy HI-ART system.
IGRT, or image guided radiation therapy, is a new form of radiotherapy using X-ray imaging during treatments to locate and focus dosing beams more precisely on tumors. IGRT brings scanning and radiation equipment together to permit the doctor to see the area of the body almost simultaneously while treating.
Prior to IGRT, physicians were unable to know the daily status of the tumor or tissues. With IGRT, more frequent imaging just prior to daily treatment enables physicians to pinpoint the position of the tumor and the surrounding normal tissues just as they are at time of treatment. With these more defined targets, patients can receive higher, more precise doses of radiation for better control of cancer and minimal effect to surrounding, normal tissues.
IGRT also enables doctors to make real-time adaptations to the treatment plan. The high-quality images of the tumor or treatment area obtained at the time of treatment allow clinicians to quickly reposition the patient as needed on the table. 3-D cone beam CT images give clinicians a clear view of the tumor site and surrounding bones, organs and soft tissue. With IGRT, radiation oncologists no longer need to treat a relatively large margin of healthy tissue around the tumor, but can minimize the amount of healthy tissue exposed to the treatment beam.
IGRT is suitable for some diagnoses, cancers and patients, but not all.
One of the first locations in the Sacramento Valley to offer Stereotactic Body Radiation Therapy (SBRT), the Department of Radiation Oncology at UC Davis Comprehensive Cancer Center has provided this high-tech treatment for more than 10 years.
Stereotactic body radiation therapy (SBRT) is a similar procedure to brain stereotactic radiosurgery and radiotherapy (see Gamma Knife), except it is used on tumors outside the brain (extracranial), generally in the lungs, liver and spine. SBRT is an emerging treatment for lung cancer in patients who are not candidates for surgery.
SBRT uses highly accurate imaging to deliver precise, high dose radiation (either in a single dose or in a small number of high-dose fractions) to areas with substantial normal organ motion inside the body. SBRT involves patient immobilization and image-guided radiation therapy (IGRT). The technologically advanced imaging techniques used in this treatment can predict tumor motion and guide the dose to the tumor site, ensuring safe and effective cancer treatment.
The Department of Radiation Oncology uses the new Elekta-S linear accelerator as it safely and effectively delivers highly focal radiation treatments to a larger target.
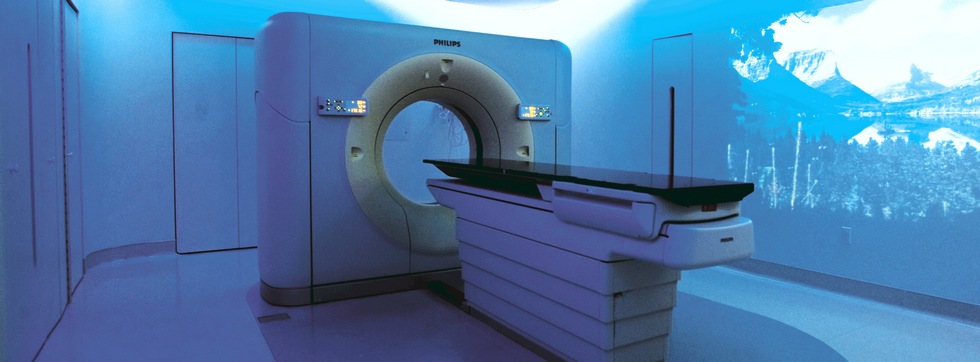
 CT simulation is a procedure used during the treatment planning stage to identify the exact location and size of the area that needs treatment.
CT simulation is a procedure used during the treatment planning stage to identify the exact location and size of the area that needs treatment.
UC Davis uses a state-of-the-art CT scanner capable of producing real-time, digitally reconstructed radiographs (DRRs). This advanced machine allows the clinician to perform a virtual simulation on a CT dataset based on each patient's unique anatomy. It is a volumetric simulation that takes into account every curve and angle of the individual, allowing each tumor to be accurately outlined and the beam(s) of radiation set to the center of the tumor.
 This focus on patient uniqueness establishes CT simulation as an essential tool for conformal radiation therapy, and allows for minimization of normal tissue volume treated. In addition to enhanced visualization of the patient’s anatomy, CT simulation can be linked to other scan technology to achieve an even higher level of visualization.
This focus on patient uniqueness establishes CT simulation as an essential tool for conformal radiation therapy, and allows for minimization of normal tissue volume treated. In addition to enhanced visualization of the patient’s anatomy, CT simulation can be linked to other scan technology to achieve an even higher level of visualization.
Patients coming to UC Davis are fortunate to be able to experience the latest CT simulation technology — a new, high-tech CT suite called the Ambient Experience that combines advanced treatment with an environment that is more positive for the patient. With Ambient Experience, patient comfort is at the forefront. A four-dimensional simulator provides precise information, taking into account the patient’s respiration cycle. Lighting, sights and sound — based on a theme chosen by each patient — are designed to calm nerves and improve delivery.
The UC Davis Department of Radiation Oncology prides itself on being a leader in providing state-of-the-art, high-tech treatment machines that give patients the best chance in their fight against cancer. The combination of the TomoTherapy, Gamma Knife, and Elekta Versa HD Blue and Gold machines at the UC Davis Health Department of Radiation Oncology means that we have broad capabilities in treating patients including, Vision RT, to support safer treatment for all patients and to patients whose options may have been limited at other institutions.
Elekta Versa Blue
Elekta Versa Blue high-definition (HD) is an innovative digital linear accelerator integrated with a suite of advanced imaging tools specifically designed for image guided radiation therapy (IGRT). Versa Blue comes from years of research. It was produced in response to the challenges associated with precision in radiation therapy. Versa Blue technology allows clinicians to address set-up challenges and organ motion issues. It helps reduce margins, increase dose and improve outcomes for many patients treated at the UC Davis Comprehensive Cancer Center.
Elekta Versa Gold
Elekta Versa Gold high-definition (HD) is the newest linear accelerator at UC Davis. Versa Gold combines a linear accelerator with an integrated 3-D volume imaging system that allows physicians to visualize the target at the time and point of treatment. With this new technology, UC Davis has three advanced machines capable of image guided radiotherapy (IGRT) and intensity modulated radiotherapy (IMRT). Versa Gold uses state-of-the-art precision technology to treat tumors, lesions and malformations throughout the body, as well as sites in the brain that are not accessible to the Gamma Knife.
Since organs may shift naturally — during breathing, for example — affecting the exact location of the tumor or target, Versa Gold allows clinicians to make immediate adjustments in the patient's position to ensure that the radiation dose hits its precise target and little of the surrounding healthy tissue. The ability to make necessary changes at the time of treatment is also an advantage because the tumor may have changed shape or size since a previous treatment. The precise nature of Versa Gold means that many patients who were not candidates for older methods of radiation therapy may now receive treatment.
Gamma Knife
The Leksell Gamma Knife is a highly precise tool used to target small tumors or neural tissues in the brain. This procedure focuses radiation to specific targets in the brain, preserving the surrounding, healthy tissue. The treatment is so precise that it if often called Gamma Knife “surgery,” but no surgical incisions are made. It is both non-invasive and painless. UC Davis was one of the first facilities to offer this sophisticated treatment, and has performed several hundred Gamma Knife surgeries over the past decade.
Radixact
The Department of Radiation Oncology is preparing to launch the Radixact radiotherapy machine in January 2026, marking a significant advancement in treatment capabilities.