Medical Physics
 The physics section is proud to support the clinicians in radiation oncology, as well as other departments, in clinical research efforts that optimize technology for simulating, planning and delivery radiation therapy, and developing new, novel, and emerging approaches in patient treatments. Several of the physicists are also faculty of the Biomedical Engineering Graduate Group, and have collaborated on publicly funded grants and/or industry relationships that provide for a wide range of opportunities for on-going research.
The physics section is proud to support the clinicians in radiation oncology, as well as other departments, in clinical research efforts that optimize technology for simulating, planning and delivery radiation therapy, and developing new, novel, and emerging approaches in patient treatments. Several of the physicists are also faculty of the Biomedical Engineering Graduate Group, and have collaborated on publicly funded grants and/or industry relationships that provide for a wide range of opportunities for on-going research.
A brief listing of some of the translational and technological development research interests within the physics section include:
- Treatment Planning Systems (TPS) based on biological and functional indices
- Image guided brachytherapy (IGBT) for optimal applicator placement, and “scan-plan-and treat” expedited delivery
- Co-registration imaging tools to optimize radiation therapy planning for the accurate determination of tumor and target margins and critical organs at risk (OAR), including the use of MRI-PET, PET-CT, and SPECT-CT
- 3D printed technology for optimized patient immpbolization and tissue compensation for highly customized (personalized) RT Delivery
- Developing highly reliable Quality Assurance (QA) technology and procedures for linac machine monitoring and patient specific QA
- Employing Machine Learning as an AI strategy to improve anatomical segmentation, treatment planning, and outcomes analysis
Research Faculty
 Sonja Dieterich
Sonja Dieterich
Sonja Dieterich, Ph.D., M.B.A.
Director, Physics Residency
Professor
Sonja Dieterich's research is focused on veterinary radiation oncology physics applications including in-vivo dosimetry with electronic portal imaging devices (EPID), scintillators and the impact of image guided radiation therapy (IGRT) on the accuracy of treatment delivery for companion animals. In human radiation oncology, Dieterich is working on an NLP-based decision support solution to improve implementation of state-of-the-art treatment approaches into daily clinical practice for rural and developing communities. She is also interested in statistical process control as a quality and safety improvement tool.
 Peter Park
Peter Park
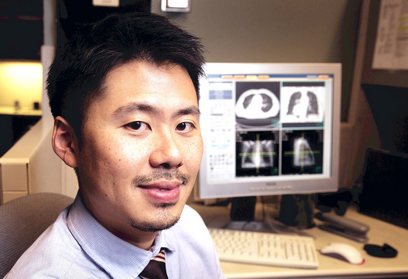
Peter Park, Ph.D., D.A.B.R.
Associate Professor
Peter Park's research is focused on diagnosis and treatment of gastrointestinal (GI) related cancer using novel imaging and image processing method to improve early detection, classification, and accurate targeting of tumor through image guided radiation therapy (IGRT). In particular, Park is interested in quantitative processing of multiphasic and multimodal images from CT and MRI to improve detection and classification of liver and pancreatic diseases. His secondary interest is in development of integrating functional imaging such as SPECT and PET in the radiation treatment planning process for GI cancer.
 Julian Perks
Julian Perks
Julian Perks, Ph.D.
Associate Director, Physics Residency
Professor
The research of Julian Perks focuses on improving patient care, quality assurance and safety through the introduction of new technologies into clinical practice. Perks works closely with the UC Davis biomedical engineering department on a number of projects. Most recently, he has implemented 3D printing technology in both our clinical workflows and research development. 3D printing has been used to enhance head and neck treatments by creating customized bolus structures to exactly match the radiation field to the patient’s external shape, including such complex anatomy as the external ear. In the arena of translational research, 3D printing has also been used to precisely calibrate the small animal model, which facilitated a key part of an immunotherapy drug development.
 Tokihiro Yamamoto
Tokihiro Yamamoto
Tokihiro Yamamoto, Ph.D.
Professor
Tokihiro Yamamoto's research is focused on development and investigation of advanced imaging technologies for treatment planning and response assessment to improve the therapeutic ratio in radiotherapy. His projects include early phase clinical trials for lung cancer: 1) CT ventilation image-guided functional avoidance radiotherapy, an emerging treatment strategy that has the potential to reduce pulmonary toxicity; and 2) a novel approach to total-lung perfusion imaging with FDG and the world’s first total-body PET/CT scanner (EXPLORER).


