School of Medicine Office of Research Newsletter
Volume 1.4 - July 2022

Message from the Associate Dean for Research
 Greetings from the School of Medicine Office of Research; we hope you are having a wonderful summer! We are marking the end of Fiscal Year 2022 by looking back at just a few of the remarkable accomplishments of our researchers.
Greetings from the School of Medicine Office of Research; we hope you are having a wonderful summer! We are marking the end of Fiscal Year 2022 by looking back at just a few of the remarkable accomplishments of our researchers.
We started FY 2021 with an increase in extramural funding over the prior year. This increased funding helped to boost the School of Medicine’s national research profile. More importantly, the overall growth in research translated into positive impact for our community. I highlight here only two of many possible examples.
The Center for Women’s Cardiovascular and Brain Health, one of four programs funded as part of the $24 million Krueger v. Wyeth cy pres settlement award, opened in May under the leadership of Professor Amparo Villablanca. The Center will include the work of cardiovascular, bioinformatics and computational scientists as well as neuropathologists and behavioral and population health scientists, while providing clinical care to women of underserved populations in our community.
The Oak Park Lawrence J. Ellison Musculoskeletal Research Center opened on June 6. The center is a new home for a material testing laboratory, cell and molecular biology facilities, tissue culture facilities, microscopy laboratory, microsurgery suite and computing facilities.
There have also been some notable awards for research teams this year. Sergio Aguilar-Gaxiola, professor of clinical internal medicine, led a team from the Center for Reducing Health Disparities and the Clinical and Translational Science Center on an interdisciplinary project in mental health for underserved communities in Solano County, and was recognized by the AAMC as an exemplar of community-engaged participatory research. Alicia Agnoli, assistant professor of family and community medicine, received the prestigious designation of a Top Ten research achievement award as well as a Distinguished Clinical Research Achievement Award (Top 3) by the Clinical Research Forum for her work on adverse effects of rapid opioid tapering, which was published in JAMA.
This is just a brief glimpse of our exciting year in SOM research. We continue forward with the support of our leadership, including Interim SOM Dean Susan Murin and Vice Dean for Research, Kim Barrett, who have brought new energy to our efforts. There are also two active workgroups related to our research goals that are developing tactics to implement our strategic plan related to research. Here’s to a great year ahead!
Ted Wun, M.D., FACP
Associate Dean for Research for the School of Medicine
Director and Principal Investigator, Clinical and Translational Science Center
Chief, Division of Hematology and Oncology
Recognition

Yu-Jui Yvonne Wan, Distinguished Professor and vice chair for research in the Department of Pathology and Laboratory Medicine, has received an approval from the PREVENT Program funded by the National Cancer Institute for her concept application. The application is entitled “Microbial Metabolite Mimicry, a Nano-drug for Colon Cancer Prevention.” The PREVENT program is a peer-reviewed agent development program designed to support preclinical development of innovative interventions for cancer prevention. Wan, Kit Lam, distinguished professor of biochemistry and molecular medicine, and Ruiwu Liu, research professor of chemistry in the Department of Biochemistry and Molecular Medicine, have a patent pending on this novel drug. The drug’s design is based on the shortage of metabolites directly or indirectly produced by gut microbes found in specimens obtained from colorectal cancer patients.
Congratulations to Jennifer Rosenthal, associate professor of pediatrics, and collaborators Kristin Hoffman, associate professor of neonatology, and Daniel Stein, Epic telehealth supervisor at UC Davis Health. This team received the AAMC Telehealth Equity Catalyst award on behalf of UC Davis Health. They were recognized for the innovation of UC Davis Health’s NICU Virtual Family-Centered Rounds (FCR) program and the integration of video translation services into the telehealth platform known as Extended Care.
Jan Nolta, professor in the Department of Cell Biology and Human Anatomy and Internal Medicine, received the Chancellor’s Lifetime Achievement Award in Innovation. This award recognizes researchers whose career accomplishments include innovations leading to a long-term positive impact on the lives of others and who are an inspiring influence for other innovators. Nolta serves as the director of the Stem Cell Program and the UC Davis Gene Therapy Center in the Institute for Regenerative Cures at UC Davis Health.
Congratulations to Jonathon Ross, who was appointed by Governor Newsom in June to the State Board of Optometry, which oversees licensing and regulation of the state’s Optometry and Opticianry practices. Ross has served as principal optometrist in the department of Ophthalmology and Vision Science since 2017. He previously served as an associate optometrist at Doctors Chan, Moon & Associates from 2015 to 2017. He is a past president of the Sacramento Valley Optometric Society and diplomate for the American Board of Optometry.
Impactful Publications

Willis Bowman, fellow in the Pulmonary and Critical Care program, is the first author of an article published in the June 2022 Lancet Respiratory Medicine, Proteomic biomarkers of progressive fibrosing interstitial lung disease: a multicentre cohort analysis. This article details a study in which a proteomic analysis was used to identify novel plasma biomarkers of progressive fibrosing interstitial lung disease and develop a proteomic signature to predict this phenotype. Several of Bowman’s colleagues in the division of Pulmonary and Critical care are co-authors of this study, including project scientist Angela Linderholm, fellow Janelle Vu Pugashetti, junior specialist Vivian Vo, clinical research coordinator Gabrielle Echt, resident William Leon, and assistant professor Justin Oldham.
Our faculty publish their findings in peer-reviewed “high-impact” journals - those considered to be highly influential in their fields. A journal’s impact factor is a measure of the frequency with which an average article in a journal has been cited in a particular year. The impact factor of a journal is an index number calculated by Clarivate and frequently used as a proxy for the importance of the journal in its field.
Get to Know SOMOR
The SOMOR Grants Facilitation Unit (GFU) provides high-quality support to UC Davis School of Medicine investigators in developing, writing/editing, and finalizing grant proposals to fund their research programs. The GFU assists investigators with numerous types of NIH mechanisms, including fellowship (F) awards for predoctoral and postdoctoral scholars, career development (K) awards for early-stage investigators, R-series awards (R03, R21, R01) for early stage or established investigators, and institutional training grants (T32, K12) or center grants (P or U series) for multi-investigator teams. The GFU also supports applications to a diverse range of foundations and national research funding institutions.
The GFU assists in grant development across the spectrum of complexity. The team provides strategy consultations, on-going support, and critical review. Involvement with an individual grant follows the cycle of submission until funded, which may require at least 18 months. When applications are not funded, the GFU assists in reviewing summary statements and designing a resubmission strategy. The GFU monitors national initiatives, reviews funding announcements, and interprets agency policy issues. It also follows updates to funding announcements, particularly within NIH, where individual Institutes add their own interpretations to policy coming from the NIH Office of the Director.
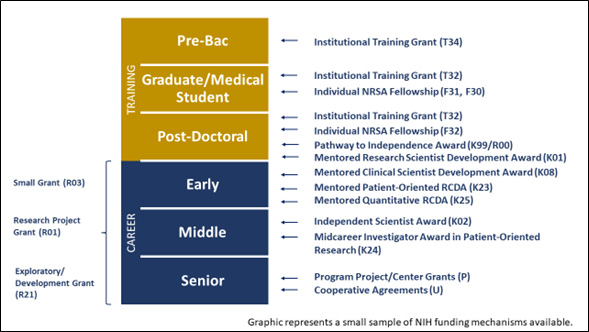
Funding mechanisms by career level.
The GFU team, led by Erica Chédin, is focused on three areas of emphasis: 1) Early Stage Investigators and Career Development (Hardeep Obhi); 2) Multi-Investigator Program Projects and Center Grants (Jeff Engler); and 3) NIH R-Series Awards and Institutional Training Grants (Heather Hughes, starting July 24). The highly collaborative and integrated GFU team continually share best practices and lessons learned to best support SOM investigators.
In addition to offering individualized proposal support, the GFU also provides mentoring and instruction in grant writing to investigators across UC Davis SOM via formal courses and invited lectureship. The GFU team provides instruction to various programs, department, classes, and clubs on effective proposal writing. Notably, the GFU has collaborated for over 10 years with lead instructor Sally Ozonoff to develop a two-quarter grant writing course required for institutionally funded scholars (e.g., CTSC KL2 and TL1 program and others).
The Introduction to Grant Writing I and II courses (CLH 208 and 209, 4 units) lead scholars through the required components of NIH grant proposals. Classes include lecture time and break-out sessions into small writing groups, each led by an instructor. Scholars are introduced to individual grant components during lecture and led through the writing these sections.
An advantage of this class is that scholars gain reviewer experience, and their reviewer assignments change across sessions. This provides scholars with the opportunity to be a reviewer and receive useful peer reviews. At the end of the 20-week course, there is a mock study session where they review completed proposals from a different small writing group, ensuring this is the first time that the reviewer sees the proposal. This invaluable experience allows scholars to participate in an NIH-style study section and complete review summary sheets with scores using NIH review criteria.
SOMOR Grant Facilitation Unit
Erica Chédin, Ph.D.
Director
emchedin@ucdavis.edu
Hardeep Obhi, Ph.D.
Research Development Specialist
hkobhi@ucdavis.edu
Jeff Engler, Ph.D.
Research Development Specialist
jaengler@ucdavis.edu
Heather Hughes, Ph.D.
Research Development Specialist
hkahughes@ucdavis.edu
Feature: UC Davis Cleft and Craniofacial Team
 July is National Cleft and Craniofacial Awareness and Prevention Month, a time to raise awareness and improve understanding of children with craniofacial differences. UC Davis Children’s Hospital’s Cleft and Craniofacial Team, co-led by Craig Senders, professor emeritus of pediatric otolaryngology, and Travis Tollefson, professor and division chief of facial plastic and reconstructive surgery is a patient-centered group of interdisciplinary professionals providing care to these children.
July is National Cleft and Craniofacial Awareness and Prevention Month, a time to raise awareness and improve understanding of children with craniofacial differences. UC Davis Children’s Hospital’s Cleft and Craniofacial Team, co-led by Craig Senders, professor emeritus of pediatric otolaryngology, and Travis Tollefson, professor and division chief of facial plastic and reconstructive surgery is a patient-centered group of interdisciplinary professionals providing care to these children.
Some of the more common craniofacial differences in patients include children born with clefts of the lip and palate and other conditions of the head, face and neck. Each year in the United States, approximately 2,600 babies are born with a cleft palate and 4,400 babies are born with a cleft lip, with or without a cleft palate. Children with cleft or other craniofacial differences may need special care in areas such as early feeding, speech instruction and socialization. This care is ideally provided by interdisciplinary teams from infancy to young adulthood. Comprehensive care includes nutrition specialists, speech-language pathologists, orthodontists, otolaryngologists and surgical teams.
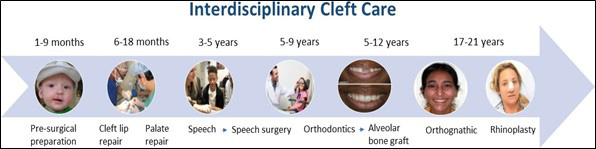
A sample timeline of the course of care for patients from birth through adulthood.
The UC Davis Cleft and Craniofacial Team includes these specialists and offers comprehensive, interdisciplinary care to patients with cleft and craniofacial problems. More importantly, explains Tollefson, the team emphasizes ongoing support to patients and their families. Since the beginning of the pandemic, Christy Roth, program coordinator, and Adebola Olarewaju, nurse practitioner, have done extra work with families to provide regular social support. The team also has an ongoing quality improvement project, in which Spanish-speaking medical students validate the forms of primarily-Spanish-speaking parents, ensuring that their concerns are properly understood and addressed by the team.
“It’s all about the kids and their parents, making sure that they are cared for,” says Tollefson about the team. “The person who makes it all work in our pediatric multidisciplinary teams is an incredible person, Kathy Porter, our cleft team coordinator.” Porter, Pediatric Special Programs Coordinator, explains that she feels her role with the craniofacial team is that of a patient advocate. “I love helping families navigate the intricacies and complexity of the medical field. The families can spend years - even decades - with our providers and services and I want to ensure it is as seamless and stress free as possible.”
|
Read More In a review of Wonder (both book and film versions) for JAMA Network, Travis Tollefson explores what patients who have physical differences that read as “otherness” to the outside world can teach us about the human condition. https://jamanetwork.com/journals/ jama/article-abstract/2670101
|
The faculty of the UC Davis Cleft and Craniofacial Reconstruction Program conduct research on the prevention and treatment of cleft and craniofacial issues. Tollefson notes that there are many exciting projects currently being conducted by the team.
One project, funded by a grant from the March of Dimes, will study the use of folic acid to decrease the incidence of cleft lip and palate. This will be a multicenter study, in which UC San Francisco and UC Davis will partner to determine the effectiveness of folic acid in preventing cleft lip or palate.
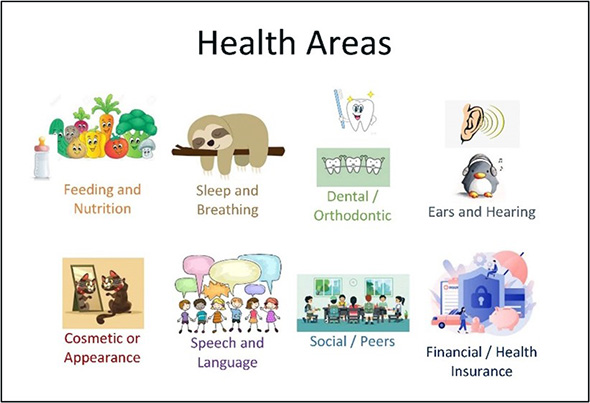 Jamie Funamura, chief of pediatric otolaryngology, is working on an ongoing research project examining the varying health priorities at different ages for children with cleft lip and/or palate from the patients’ and families’ perspectives. The goal is for multidisciplinary teams to better understand how to provide the best patient and family- centered care.
Jamie Funamura, chief of pediatric otolaryngology, is working on an ongoing research project examining the varying health priorities at different ages for children with cleft lip and/or palate from the patients’ and families’ perspectives. The goal is for multidisciplinary teams to better understand how to provide the best patient and family- centered care.
Tollefson and Roth have joined an exciting new study on the shape of muscles in the palate after surgical correction. This study will use a novel MRI that allows the 4–5-year-old child to have headphones and goggles on while the cleft team speech pathologist prompts them to speak. The MRI images are then interpreted to choose the best speech surgery for the child.
Tollefson, Roth, Olarewaju and UC Davis Pediatric Pulmonologist, Rory Kamerman-Kretzmer are key contributors to a group of cleft team professionals called Stakeholder Alliance for Children with Robin Sequence (StARS): Building Capacity for PCORI (Patient Centered Outcomes Research). They have enlisted parents and experts to better define strategies to improve care for children born with Robin Sequence.
Meet the Team
Craig W. Senders, M.D., FACS
Pediatric Otolaryngology Cleft & Craniofacial Program Co-Director
Travis T. Tollefson, M.D., M.P.H., FACS
Facial Plastic and Reconstructive Surgery Cleft & Craniofacial Program Co-Director
Christy Roth, M.S., CCC-SLP
Cleft & Craniofacial Program Coordinator
Madelena Martin, M.D.
Pediatric Geneticist
Robert S. Byrd, M.D., M.P.H.
Pediatrician
Adebola Olarewaju, M.S.N., P.N.P., Ph.D.
Nurse Practitioner
Audrey Bracchi, Au.D., F-AAA
Audiologist
Samantha McKinney, A.uD., F-AAA
Audiologist
Chuen Chie Chiang, D.D.S., M.S.
Orthodontist
Editorial: Dobbs Decision
“A woman’s right to ultimately decide if and when she becomes pregnant is the cornerstone of her ability to achieve what she desires in life for herself and her family.” – Mitchell Creinin
On June 24, the US Supreme Court ruled for the defendant in Dobbs v. Jackson Women’s Health Care Organization, reversing two landmark contraceptive cases, including Roe v. Wade, which protected abortion access in this country for fifty years. Abortion access across the country has begun to fall under newly adopted state regulations and an uncertain legal landscape threatens the work of medical professionals both in clinical practice and research.
Mitchell Creinin, professor and director of the Complex Family Planning Fellowship in the Department of Obstetrics and Gynecology, notes that it is vital that abortion research continue to be supported by the academic community. “Abortion is not just about a person deciding that she is pregnant at a time that is not ideal in her life,” he says. “Abortion is also the care we provide for people with desired pregnancies who have medical conditions that risk their lives or have pregnancies with significant fetal abnormalities or are incompatible with the ability to survive outside of the uterus. Forcing patients to endure an unnecessary risk, including when continuing the pregnancy cannot result in a viable newborn, is inhumane.”
Creinin has been conducting abortion research for more than 30 years, including developing medical abortion regimens pre-mifepristone, being an investigator in the initial US pivotal trial of mifepristone and misoprostol for medical abortion, and recent studies related to pharmacist provision of mifepristone. He has authored more than 300 peer-review papers, review articles, book chapters and books related to family planning.
As a member of the editorial board for Contraception, a leading journal for abortion research, Creinin helped craft that journal’s editorial response to the Dobbs ruling, noting that the Roe decision “improved the lives of women, families, and society as a whole, as decades of quality scientific research have demonstrated.” Further, the editorial notes that by returning reproductive rights decisions to the individual states, the Court “has decided that reproductive rights are entirely political, and should be decided by state legislatures; thus, women’s lives are now even more subject to the whims of politics.” The editorial also points out that the impact of the decision will be most heavily borne by those who already experience poor access to medical care.
“Not only is it important to offer abortion services when personally and medically needed,” Creinin adds, “but it is important for the medical community to continue to research the best ways in which we can safely and effectively provide this important health care for women and their families.”

