Alison Chan, DO, Pathology Resident
Anna Romanelli, PhD, Medical Director of Clinical Microbiology Laboratory
Introduction:
In every patient with a suspected infection, the prompt detection and identification of the organism is of utmost importance. The UC Davis Microbiology Lab offers several laboratory tests to identify the infectious organism, which ultimately guides clinicians to initiate the appropriate treatment to the patient [1]. Commonly, several routine tests are ordered upon the initial patient encounter, such as complete blood counts, chemistry panels, routine blood cultures, as well as fungal blood cultures. When a fungal blood culture is requested, a fungal Isolator tube is required to collect the blood for special lab processing. Since this lab test may be inappropriately ordered, the fungal blood culture requires the approval from the Director of Clinical Microbiology Laboratory or a Pathology resident in order to receive the fungal Isolator tube to complete the lab test. We will review the tests currently available to detect fungemia and when a fungal blood culture request is appropriate.
Lab Best Practice:
The best test to order in a patient with a bloodstream infection is a routine blood culture, which includes one anaerobic and one aerobic bottle. Routine blood culture can easily recover aerobic and anaerobic bacterial organisms as well as Candida spp., Aspergillus spp. and sometimes Fusarium spp. which are the most common fungal organisms to cause bloodstream infections. The Candida spp. is the most common invasive fungal disease and is also the fourth most common cause of blood stream infections [2]. The incidence of invasive Candidiasis also exceeds that of invasive Aspergillus and Mucormycosis [3]. This means that most fungemia can be detected using routine blood cultures.
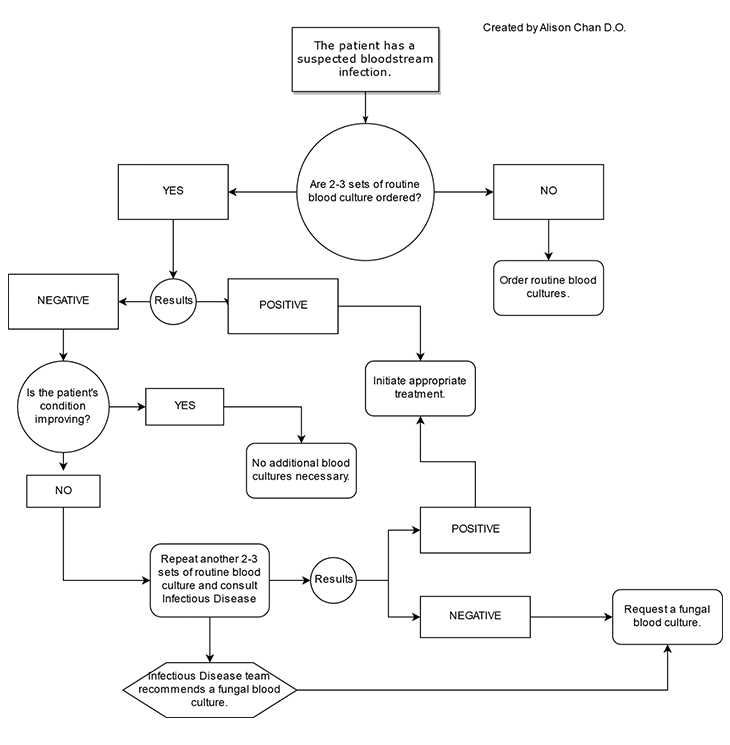
If you suspect your patient has a bloodstream infection, it is ALWAYS recommended to collect 2-3 routine blood culture sets from separate venipuncture sites and submit them to the UCDMC microbiology laboratory. Collecting multiple blood culture sets is important because it will later help you, the clinician, determine whether a reported organism is a true pathogen or a possible contaminant. If the initial 2-3 routine blood culture sets are negative, it is recommended to collect another 2-3 routine blood culture sets, again from separate venipuncture sites, such as one from each arm. The rationale is that the infectious organism, bacterial or fungal, is often recovered by the routine blood culture. At UCDMC, the BACTEC blood culture instrument incubates and checks each blood culture bottle every 10 minutes for a positive culture for a total duration of 5 days. The BACTEC instrument will alarm once a blood culture has become positive, with the Gram stain results promptly reported by the microbiology technician to the clinician. If no growth is detected after 5 days of incubation, the culture will be reported as a negative. Additionally, a consultation with the Infectious Disease team is STRONGLY recommended prior to a fungal blood culture request. Therefore, once a patient has had several negative blood culture sets, no clinical improvement, and a consultation with the Infectious Disease team is complete, the use of a fungal blood culture can be then considered.
The fungal blood culture is rarely used as the first line for diagnosing a patient with any possible fungal infection. The fungal Isolator tube is reserved for patients with suspected sepsis from the following fungi: Blastomyces dermatitidis, Coiccidioides immitis, Histoplasma capsulatum, Malessezia species, other filamentous fungi that are not recovered from routine blood cultures [4,5]. A comparison of fungi recovery between the routine blood culture and Isolator fungal tubes, showed that the Isolator fungal tubes had a higher sensitivity for detecting fungemia from the fungal organisms listed above [3].
A list of situations where a fungal blood culture is likely to be approved is provided below:
- A patient has had multiple negative routine blood culture sets and the patient has shown little to no improvement.
- The patient is immunocompromised.
- The patient has a history of fungemia.
- The patient is on total parenteral nutrition (TPN).
- It has been reported that Malassezia sepsis can occur in patients receiving TPN [8].
The following algorithm can be used when encountering a patient with a suspected bloodstream infection.
Understanding the limitations to every laboratory test is important. A study by Kosmin and Fekete, showed that the fungal Isolator tube may not perform better than a routine blood culture for the detection of fungemia in patients. Another limitation is that there is a higher contamination rate (10-12%) from the additional manual labor needed to perform the test, which may lead to more false positives [10].
Other laboratory tests available in-house at UC Davis, are MALDI-TOF identification for Candida spp., and the standard fungal culture with morphologic identification for all other fungi. If needed, the fungal isolate can be sent to the University of Texas Health Science Center at San Antonio Fungus Testing Laboratory for 18S rRNA PCR identification. Additional send-out laboratory tests include the Aspergillus Galactomannan Antigen by EIA and (1,3)-beta-D-glucan tests which are performed at ARUP Laboratories.
As with all lab tests, a negative result will not rule out a potential fungal infection. A positive result should always be correlated with a patient's clinical situation because of the possible false-positives. In situations where a patient's condition does not improve, repeat testing can be performed if a fungal infection is still highly suspected.
Bottom Line:
The approval of a fungal blood culture is done on a case-by-case basis. A patient with a suspected bloodstream infection is recommended to have 2-3 routine blood culture sets collected FIRST from different venipuncture sites. If these blood culture sets are negative after 5 days and the patient's condition does not improve, repeat another 2-3 sets of routine blood cultures and consult the Infectious Disease team for further guidance. Once these steps are completed, a fungal blood culture request will likely be approved. However, if a clinician highly suspects a specific fungal infection, that is not recovered with a routine blood culture, a fungal blood culture could be approved earlier.
References:
- Murray PR, Masure H. Current approaches to the diagnosis of bacterial and fungal bloodstream infections for ICU. Crit Care Med. 2012 Dec;40(12):3277-3282.
- Azap, Ozlem K.; Ergönül, Önder. Chapter 12 – Antifungal Stewardship. Antimicrobial Stewardship: Developments in Emerging and Existing Infectious Diseases. 2017; 147-163.
- Guinea, J. Global trends in the distribution of Candida species causing candidemia. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2014; 20(6):5-10.
- Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010;23(2):367-81.
- Telenti A, Roberts GD. Fungal blood cultures. Eur. J. Clin. Microbiol. Infect. Dis., 1989 Sep;8(9):825-831.
- Lyon R, Wood G. Comparison of the BacT/Alert and isolator bood culture systems for recovery of fungi. American Journal of Clinical Pathology. 1995 Mar; 103(5): 660-662.
- Zheng S, Ng TY, Li H, Tan AL, Tan TT, Tan BH. A dedicated fungal culture medium is useful in the diagnosis of fungemia: a retrospective cross-sectional study. Plos One. 2016 Oct. https://doi.org/10.1371/journal.pone.0164668. Accessed 10/9/18.
- Shparago N.I., Bruno P.P., Bennett J. Systemic Malassezia furfur infection in an adult receiving total parenteral nutrition. J Am Osteopath Assoc. 1995 Jun; 95(6): 375–377.
- Kosmin AR, Fekete T. Use of fungal blood cultures in an academic medical center. Journal of Clinical Microbiology. 2008 Nov.; 46(11)3800-3801.
- Geha DJ, Robert GD. Laboratory detection of fungemia. Clin Lab Med. 1994 Mar;14(1):83-97.



