Luke Dang, M.D., Scott Bainbridge, C.L.S., Nam Tran, Ph.D.
Introduction
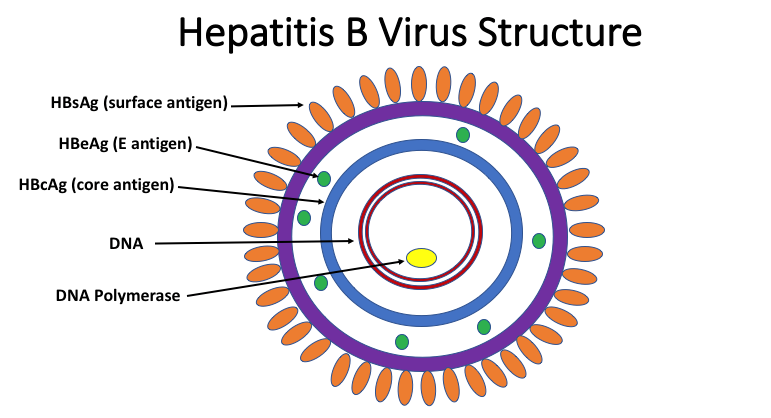
Hepatitis B virus (HBV) was first discovered in 1965. Briefly, HBV is a DNA virus from the Hepadnaviridae family which is spread via contaminated body fluids(1). After exposure, the virus enters hepatocytes and integrates its circular, partially double-stranded DNA genome (3.2 kb in size) to the host cell nucleus as a covalently closed circular DNA (cccDNA) intermediate, which acts as a stable nuclear template for viral replication(2). This mechanism enables the virus to chronically infect the host and reactivate at a later date (secondary to immunocompromise as in the case of transplantation, chemotherapy, immunosuppression or infection (as in the case of HIV)). Reverse transcription of the cccDNA then results in assembly and exocytosis of new viral particles. Hepatitis B exhibits geographic variation and is classified into 9 genotypes (A-I), with some differences in disease manifestations, although this remains an area of ongoing research(3).
Clinical Manifestations and Epidemiology
Hepatitis B virus infection exhibits a range of manifestations in the acute and chronic time frames(4). Acute infection can be sub-clinical or clinical in severity and can cause both icteric (~30%) or anicteric hepatitis (~70%). In a small subset of patients (~0.5%), acute infection can lead to fulminant hepatic failure secondary to immunologic lysis of the virus-infected hepatocytes. For chronically infected patients, long term exposure to viral antigens can lead to immune-mediated liver injury as well as direct viral cytotoxicity. This ongoing viral insult eventually can lead to chronic hepatitis, cirrhosis, or hepatocellular carcinoma, although other patients may remain asymptomatic carriers. The incubation period ranges from 30-120 days and is detectable within 30-60 days.
Although preventable by immunization(5), hepatitis B remains a significant worldwide cause of morbidity and mortality. The World Health Organization estimated that in 2015, 257 million individuals had chronic hepatitis B and 887,000 individuals died as a result of hepatitis B (secondary to cirrhosis and hepatocellular carcinoma)(6). In endemic areas, hepatitis B is transmitted both vertically (from mother to child at birth) and horizontally (via to infected body fluids, e.g. sexual contact or needlestick exposure). Chronic infection is more common in those infected at lower ages compared to infected adults. A subset of individuals with hepatitis B are coinfected with HIV or hepatitis D as well. Hepatitis D is a subviral agent which is dependent upon the presence of HBV for replication(7). Infection can occur coincident to HBV infection (coinfection) or subsequent to chronic or latent HBV infection (superinfection). Coinfection of hepatitis D with HBV is regarded as the most severe chronic hepatitis, although it can also be avoided via hepatitis B vaccination.
Diagnostic Serologic Testing for Hepatitis B
Since infected individuals may not display any symptoms upon infection and hepatitis B cannot be specifically identified from other viral etiologies clinically, confirmation of hepatitis B infection relies upon laboratory testing (Figure 1). Additionally, although treatment of acute infection is primarily supportive, chronically infected patients with immune active phase disease(8) or with other indications(9) may be treated with anti-viral medications. Given the severity of long-term complications of this entity (cirrhosis, HCC), appropriate identification of infected patients is a critical clinical task.
Hepatitis B screening should be performed on patients with signs and symptoms suggestive of acute or chronic hepatitis as well as asymptomatic individuals with a history of or high risk of exposure (e.g., HIV or hepatitis C infected, multiple sexual partners, history of intravenous drug use, end-stage renal disease, household contacts of known hepatitis B infected individuals, chronic liver disease, incarcerated, parents who were born in geographic areas with hepatitis B prevalence >8%) or those at high risk of complications (individuals born in countries with a high hepatitis B prevalence, pregnant women, immunocompromised patients, donors for blood or tissue products, infants born to infected mothers)(10).
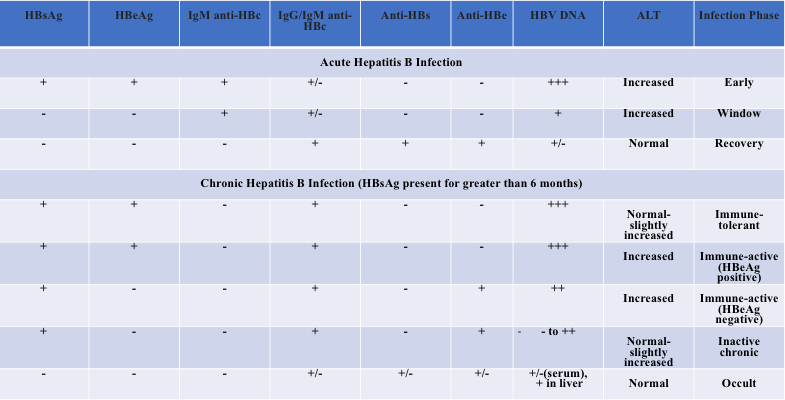
Serologic testing for multiple viral antigens and the corresponding antibodies allows for identification of both acute and chronic infections. In the setting of acute infection, hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg), and hepatitis B DNA (HBV DNA) are present, and IgM anti-HBc (antibody against the hepatitis B core antigen) appears shortly thereafter. The presence of IgM anti-HBc and HBsAg, without anti-HBsAg is diagnostic of acute infection (see Table 1 for summary of interpretation of serologic results). Recovery after acute infection is marked by the reduction of serum HBV DNA and seroconversion to anti-HBe and anti-HBs (accompanied by disappearance of HBeAg and HBsAg, although rarely HBsAg and anti-HBs may coexist (1.2% in a study by Lee et al)(11). Class switching of the IgM anti-HBc to IgG anti-HBc also occurs after initial infection. Therefore, individuals with a prior history of natural infection will have IgG anti-HBc as well as anti-HBs. Conversely, the presence of only anti-HBs without anti-HBc is indicative of a vaccinated individual. Individuals with a chronic infection may have persistent HBeAg, with continued circulation of HBsAg (and HBV DNA), with IgG but not IgM anti-HBc, without anti-HBs. Detection of HBsAg for longer than six months after acute infection is diagnostic of chronic infection. Although quantitation of serum HBV DNA may be used clinically to assess ongoing HBV replication, serum HBV DNA may be negative in inactive chronic HBV. Since recovery from acute infection is accompanied by disappearance of HBV DNA, PCR testing for quantitation of serum HBV DNA occurs more frequently in the assessment of chronic infection rather than the acute setting or during initial screening.
Table 1. Interpretation of Hepatitis B Serological Results. Adapted from UpToDate. Hepatitis B virus: Screening and diagnosis.; Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 2018; 67:1560.
Hepatitis B e Antigen and Chronic Hepatitis B Infection
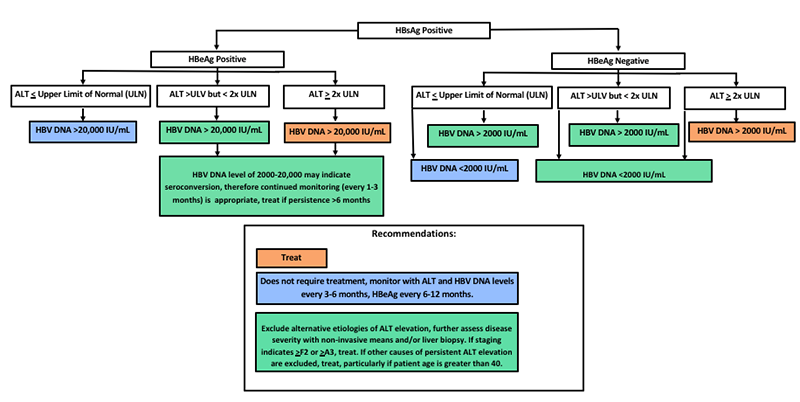
The hepatitis B e antigen (HBeAg) is a marker of replication and infectivity. In the setting of acute infection, conversion from HBeAg to anti-HBe typically occurs before the transition from HBsAg to anti-HBs. However, in the setting of chronic hepatitis B infection, seroconversion may not be observed. Chronic HBV infection is divided into multiple phases (see Figure 1 from Terrault et al)(12-13). In the immune-tolerant phase, HBeAg is positive, HBV DNA levels are high, alanine transaminase (ALT) and aspartate transaminase (AST) levels are normal to minimally elevated, and there is minimal hepatic inflammation or fibrosis. The immune-active phase is characterized by lower HBV DNA levels, with intermittently or constant ALT/AST levels, and chronic, moderate to severe hepatic inflammation (with or without fibrosis). The inactive phase has negative HBeAg, positive anti-HBe, low HBV DNA, normal AST/ALT, and absence of hepatic inflammation (variation in degree of fibrosis). The immune-active phase can be further divided by HBeAg status, and management recommendations have been made in the past based on this basis (Terrault et al, see Figure 2 below).
Occult HBV Infection and Reactivation in the Transplantation Setting
Isolated anti-HBc without HBsAg or anti-HBs can occur during acute infection when anti-HBc is primarily IgM, when anti-HBs has waned (years after recovery from natural infection), in the setting of HBsAg mutations which evade testing or with low titers of HBsAg which are below testing threshold cutoffs. Testing for anti-HBc can also help detect patients with occult infection, that is, patients with detectable HBV DNA by PCR but who are HBsAg seronegative. These patients may have low serum HBV DNA levels, however transplantation of livers from these individuals may result in infection upon transplantation(14). Additionally, patients with occult hepatic infection may experience reinfection upon receipt of immunosuppressive regimens as in the case of bone marrow or stem cell transplant(15). Therefore, diligent hepatitis B screening of patients during transplantation evaluation is appropriate. Patients positive for HBsAg and HBeAg are at higher risk for reactivation in the transplant setting(16-17).
Testing Platform at UC Davis Health
The UC Davis Health Hepatitis B e antigen and antibody test are now performed on the Diasorin Liason XL instrument on serum or plasma samples – providing faster turnaround times and exhibiting excellent clinical performance.
References
- Castaneda D, Gonzalez AJ, Alomari M, Tandon K, Zervos XB. From hepatitis A to E: A critical review of viral hepatitis. World J Gastroenterol. 2021 Apr 28;27(16):1691-1715.
- Rybicka M, Bielawski KP. Recent Advances in Understanding, Diagnosing, and Treating Hepatitis B Virus Infection. Microorganisms. 2020; 8.
- Revill PA, Tu T, Netter HJ, Yuen LKW, Locarnini SA, Littlejohn M. The evolution and clinical impact of hepatitis B virus genome diversity. Nat Rev Gastroenterol Hepatol. 2020;17:618–634.
- UpToDate. Hepatitis B virus: Clinical manifestations and natural history. Accessed on May 18, 2021.
- Centers for Disease Control and Prevention. Hepatitis B. Accessed on May 18, 2021.
- World Health Organization Hepatitis B Factsheet. Accessed on May 18, 2021.
- Centers for Disease Control and Prevention. Hepatitis D. Accessed on May 18, 2021.
- European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–398.
- Jeng WJ, Lok AS. Should Treatment Indications for Chronic Hepatitis B Be Expanded? Clin Gastroenterol Hepatol. 2020.
- UpToDate. Hepatitis B virus: Screening and diagnosis. Accessed on May 18, 2021.
- Lee WM, King WC, Schwarz KB, Rule J, Lok ASF; HBRN Investigators. Prevalence and clinical features of patients with concurrent HBsAg and anti-HBs: Evaluation of the hepatitis B research network cohort. J Viral Hepat. 2020 Sep;27(9):922-931.
- Croagh CM, Lubel JS. Natural history of chronic hepatitis B: phases in a complex relationship. World J Gastroenterol. 2014;20:10395–10404.
- Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 2018; 67:1560.
- Dickson RC, Everhart JE, Lake JR, Wei Y, Seaberg EC, Wiesner RH, Zetterman RK, Pruett TL, Ishitani MB, Hoofnagle JH. Transmission of hepatitis B by transplantation of livers from donors positive for antibody to hepatitis B core antigen. The National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. Gastroenterology. 1997 Nov;113(5):1668-74.
- UpToDate. Hepatitis B virus reactivation associated with immunosuppressive therapy. Accessed on May 18, 2021.
- Dhédin N, Douvin C, Kuentz M, Saint Marc MF, Reman O, Rieux C, Bernaudin F, Norol F, Cordonnier C, Bobin D, Metreau JM, Vernant JP. Reverse seroconversion of hepatitis B after allogeneic bone marrow transplantation: a retrospective study of 37 patients with pretransplant anti-HBs and anti-HBc. Transplantation. 1998 Sep 15;66(5):616-9.
- Lau GK, Leung YH, Fong DY, Au WY, Kwong YL, Lie A, Hou JL, Wen YM, Nanj A, Liang R. High hepatitis B virus (HBV) DNA viral load as the most important risk factor for HBV reactivation in patients positive for HBV surface antigen undergoing autologous hematopoietic cell transplantation. Blood. 2002 Apr 1;99(7):2324-30.



