Happy homecoming for local baby after high-risk heart procedures
JJ Gomez-Flores’ heart defect meant a long, scary road ahead. But he and his family would not be alone on the ride
For the Gomez-Flores family, the arrival of their son in November of 2021 was a blessing. Jesus – affectionately called “JJ” – was Victor Gomez and Sofia Flores’ first child together. He was the only boy among three older sisters ages 3, 7 and 15. The family was thrilled but also knew that JJ would face some serious health challenges ahead.
During Sofia’s pregnancy, JJ had been diagnosed with hypoplastic left heart syndrome (HLHS) at the UC Davis Fetal Care and Treatment Center. The left side of his heart had not formed properly, affecting blood flow. Survival of infants with HLHS most often requires immediate surgery and subsequent procedures. Many infants die within the first two weeks of life.
“We were so worried,” Victor Gomez-Flores said. “We knew that the surgeries to help him survive were very dangerous.”
As the family grappled with the gravity of the situation, they were referred to the UC Davis Pediatric Heart Center. The center has an integrated team of surgeons, specialists, pediatric cardiologists and nurses. They offer families, like JJ’s, the most sophisticated, specialized expertise … and that’s just what the HLHS congenital heart defect would require.
Surgery for HLHS usually is done in three separate stages. Although these surgeries do not cure the condition, surgeons are able to gradually reconstruct the heart, improving survival. The Gomez-Flores family put their trust in the UC Davis Children’s Hospital care team to save JJ’s life.
“It was going to be a long road,” Gomez-Flores said. “But without a doubt, we felt JJ was in good hands.”
Following their hearts: Trusting the care team
A baby born with this type of heart defect needs several surgeries to increase blood flow to the body and bypass the poorly functioning left side of the heart. The first is done just a few days after birth. UC Davis Children’s Hospital pediatric cardiothoracic surgeon Gary Raff performed the first surgery, known as the Norwood procedure, when JJ was six days old.

To reconstruct JJ’s heart, Raff first disconnected the pulmonary artery from the lungs. Then he rebuilt the aorta, carefully converting the aorta and the pulmonary artery to a single artery going to the body. This allowed blood flow through the coronary artery. Raff then removed the atrial septum to allow for blood to freely mix in the heart. Lastly, he placed a shunt from the right ventricle to the pulmonary arteries.
“These are always challenging operations,” Raff said. “The surgery is among the highest risk procedures done in congenital heart surgery.”
These are always challenging operations. The surgery is among the highest risk procedures done in congenital heart surgery.”—Gary Raff, pediatric cardiothoracic surgeon
Although the surgery went well, JJ’s recovery was complicated by necrotizing enterocolitis, a serious gastrointestinal problem that inflames intestinal tissue, causing it to die. A hole can form in a baby's intestine and bacteria can leak into the abdomen or bloodstream through the hole.
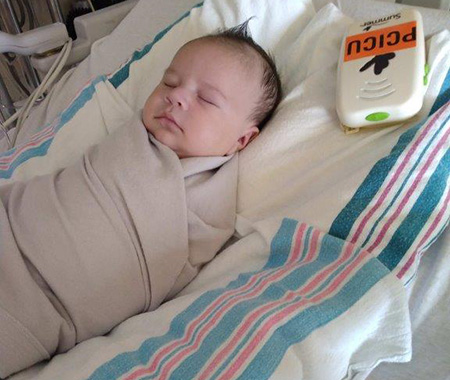
JJ spent several weeks in the Pediatric and Cardiac Intensive Care Unit (PCICU). It was a wonderful day when the baby was discharged from the hospital on December 20, 2021, just in time for Christmas. But soon, JJ’s parents’ own hearts would begin to race once again when he was readmitted to the PCICU in January 2022 for a cardiac catheterization in anticipation of the next scheduled surgery.
In good faith: Holding on for the ride

JJ had his second operation at 4 months of age. On March 8, 2022, the surgical team, led by Raff, performed a bi-directional Glenn shunt procedure. They removed the tube that connects the heart to the lungs and then redirected blood flow from the upper body veins to the lungs.
Again, the surgery went well, but JJ’s recovery would not go smoothly.
“JJ had lots of challenges,” said Virpal Donley, PICU/PCICU nurse manager at UC Davis Children’s Hospital. “By March 15, he was placed on ECMO.”
ECMO, or extracorporeal membrane oxygenation, is a form of life support for people with life-threatening illness or injury that affects the function of their heart or lungs. The machine helps to breathe for the child so their lungs can rest.
The entire team of doctors and nurses were doing all they could to save our son's life. They made their best efforts to take care of both JJ and us as parents. Despite the fear, we felt we could not be in a better place.”—Victor Gomez-Flores, JJ’s dad
JJ required ECMO because of thrombosis, or swelling and clotting of his left pulmonary artery, an unusual complication after this operation. This heart-lung machine allowed the team to stabilize JJ and then the cardiac catheterization was completed, which led to diagnosis of a blood clot in the left pulmonary artery.
JJ’s family was terrified.
“The entire team of doctors and nurses were doing all they could to save our son's life. We were scared but just kept praying,” Gomez said. “The team made their best efforts to take care of both JJ and us as parents. Despite the fear, we felt we could not be in a better place.”
Recovery takes another turn
On March 31, JJ had another heart surgery to take down the Glenn shunt since he was not improving. The family continued their vigil.
“Dr. Raff told us from the start that he would care for JJ as if he were his own son,” Gomez-Flores. “He never gave up.”

”JJ’s blood clot in the pulmonary artery was a serious problem and I told the family we would do whatever we could to get him through this,” Raff said. “I felt the best way to reduce risk was to take down the Glenn shunt which relies on passive venous blood flow and place a high-pressure shunt that would allow us time to use medicine to resolve the blood clots over time. This would also hopefully allow him to come off ECMO.”
It worked.
JJ’s chest remained open for the next five days so the team could monitor him and check for bleeding as he began to heal. It would be a long recovery, but he was back on the road. JJ would spend more than two months in the PCICU before he would be strong enough to be discharged.
“We gave JJ and his family a lot of TLC and worked hard to get him back to a baseline,” Donley said. “There were so many little victories that we held onto.”
A heartfelt celebration: JJ goes home
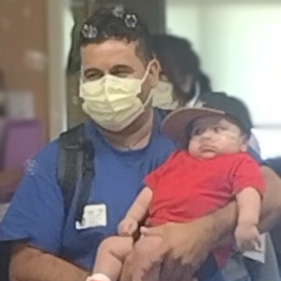
Finally, more than seven months after he was born and after more than two months in the PCICU recovering, JJ was able to leave the hospital on June 29. His care team, who had so diligently cared for JJ and his family, celebrated his last day in the hospital with a parade, complete with bubbles.
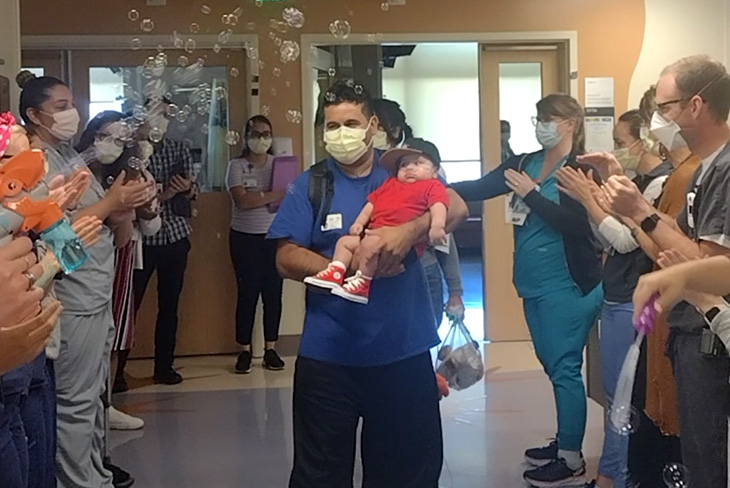
“It was amazing,” Donley said, “to watch them walk out the door. It’s why we do what we do.”
The family was so thankful for UC Davis Children’s Hospital staff.
“The whole team took such good care of us as parents while helping our son,” Gomez-Flores said. “You are incredible.”
It was amazing to watch them walk out the door. It’s why we do what we do.”—Virpal Donley, PICU/PCICU nurse manager
Grateful to be on the ride together
Now 1 year old, JJ is a very active, happy boy who enjoys playing with his toys, watching his favorite farm animal cartoons and playing with his 7-year-old sister, Alexa. JJ has follow-up visits with pediatric cardiologist, Yoni Dayan, another of the family’s heroes. At the Pediatric Cardiology Clinic, the team monitors JJ’s progress and continues to celebrate his successes.
“JJ is thriving! He has had a tough road so far, but now has been able to grow, gain weight, and live life to the fullest since his last surgery,” said Dayan. “It is always a pleasure to see JJ and his family in clinic. He is on quite a lot of medications at this time, both for heart failure and for heart rhythm control, but I am hopeful and confident that we can safely get JJ to his next stage of repair and continue his life-long congenital heart disease journey.”

The Gomez-Flores family knows that there are more surgeries ahead but is relishing the moments in between. Plus, they know when the time comes, they can be confident in the people who will be right beside them on the ride.
“We thank God for everyone at UC Davis Children’s Hospital. Thanks to you, our baby is alive and at home with his sisters,” Gomez-Flores said. “We could not be more grateful. With all the support from the hospital staff, we will get through this … together.”
We thank God for everyone at UC Davis Children’s Hospital. Thanks to you, our baby is alive and at home with his sisters. We could not be more grateful. With all the support from the hospital staff, we will get through this … together.”—Victor Gomez-Flores, JJ’s dad
UC Davis Children's Hospital is the Sacramento region's only nationally ranked, comprehensive hospital providing care for infants, children, adolescents and young adults with primary, subspecialty and critical care. It includes the Central Valley's only pediatric emergency department and level I pediatric trauma center, which offers the highest level of care for its critically ill patients, as well as a level I children’s surgery center. The 129-bed children's hospital includes the state-of-the-art 49-bed neonatal and 24-bed pediatric intensive care and pediatric cardiac intensive care units. For more information, visit children.ucdavis.edu.