Residency Program - Case of the Month
July 2012 - Presented by Mahan Matin, M.D.
Answer:
Consistent with cysticercosis
Discussion:
Neurocysticercosis develops when the larval form of the pig tapeworm Taenia solium encysts in the central nervous system, inciting a surrounding inflammatory and granulomatous response. It is the most common helminthic infection in the central nervous system and the most common cause of acquired seizures worldwide. The disease is endemic to nearly all continents, but is particularly prevalent in Mexico (where it is the leading cause of space-occupying intracranial lesions), Central and South America, India, Africa, and China. An increasing incidence in the United States is largely attributable to cases occurring in immigrants from these regions.
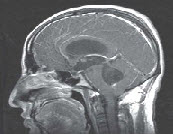
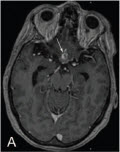
After ingestion of the egg of the tapeworm from contaminated water or undercooked meat, the egg loses its capsule when it comes into contact with the acid pH of the stomach. The larvae enter the bloodstream and spread to various organs, including the CNS. In this environment, they cannot grow to adult worms, so they remain as cysts indefinitely (Fig. 1). Initially, the cyst produces minimal response, and the infestation may remain silent for months to years. The cysts are usually found in the cerebral cortex but can occur in the meninges of the base of the brain, in the ventricles, and, rarely, in the spinal cord (Fig 2-3).
Symptoms occur when the worm dies (approximately 18 months following primary infection), the cyst ruptures, and the contents leak, producing a dense inflammatory response composed of lymphocytes, eosinophils, and plasma cells. With time, a fibrous capsule forms. Some patients are asymptomatic or have nonspecific symptoms. Epilepsy is the most common presenting symptom; other manifestations include severe episodic headache, meningitis, obstructive hydrocephalus (if the cyst is near a ventricle or the subarachnoid space), and cognitive problems.
Radiologic diagnosis is often straightforward, although the appearance varies depending on the life cycle stage of the parasite and the age of the lesion. The presence of multifocal, rim-enhancing cerebral cysts on neuroimaging studies suffices in many cases to prompt a diagnostic as well as therapeutic course of antihelmintic chemotherapy, but a substantial proportion of patients present with solitary lesions, and the host's reaction to the decaying parasite may convert the cyst to a deceptively solid inflammatory pseudotumor.
When the larvae are invading the brain, they appear as small nonenhancing edematous lesions, later forming small enhancing nodules. As the lesions become cystic and the larvae start to die, surrounding edema develops due to the inflammatory response to the cyst contents, and there is ring enhancement due to the formation of granulation tissue and a thick capsule. Usually the lesions are less than 20 mm in diameter. Solitary lesions can be difficult to distinguish from a neoplasm owing to the surrounding edema and the cyst enhancement.
It may even mimic a glioblastoma multiforme radiologically. In these cases
neurosurgical intervention may be obviated by cerebrospinal fluid or serologic assay for specific anticysticercal antibodies or antigens, but false-negative results may be encountered, especially in subjects with unifocal disease.
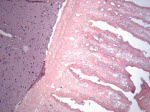
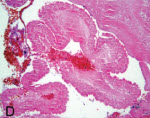
To make the definitive diagnosis histologically, one must see the parasite. The live parasite has a single scolex with four suckers and a double row of hooklets (Fig 4). The cyst wall has an outer cuticular layer, a middle pseudoepithelial cellular layer, and an inner reticular layer. However, in excisions or biopsies of cysticercus, only the cuticular layer of the dead worm is seen with H&E stain (Fig 5-6).
References:
1- Diagnostic Pathology of Infectious Disease. Richard L. Kradin, Saunders; Har/Psc edition (February 16, 2010)
2- Intracranial Lesions Mimicking Neoplasms. Cunliffe et al, Arch Pathol Lab Med—Vol 133, January 2009
3- Rosai and Ackerman's Surgical Pathology, Mosby; 10 edition
4- http://www.parasite-diagnosis.ch



 Meet our Residency Program Director
Meet our Residency Program Director
