Residency Program - Case of the Month
September 2012 - Presented by Rebecca Sonu, M.D.
Clinical history:
The patient is a 37 year-old nulligravida female with a history of abnormal menstruation and more recently, episodes of severe lower abdominal cramping and copious vaginal bleeding. She has no significant past medical history. She has a history of smoking two packs per week for 15 years. On pelvic examination, the external genitalia and vagina were normal. The cervix was dilated and effaced revealing a protruding erythematous tumor. The rectovaginal exam confirmed cervical effacement and uterine enlargement. No discrete adnexal masses were palpated. A PET/CT scan revealed a prominent hypermetabolic area along the endometrium of the uterus. No other significant hypermetabolic areas were found elsewhere in the body. The patient subsequently underwent a total abdominal hysterectomy bilateral salpingo-oophorectomy with bilateral pelvic sidewall lymph node dissection.
Gross examination:
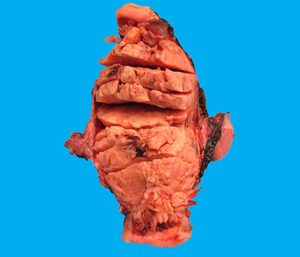
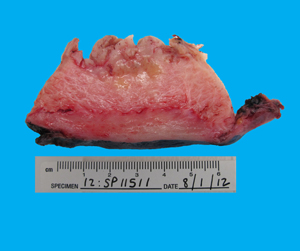
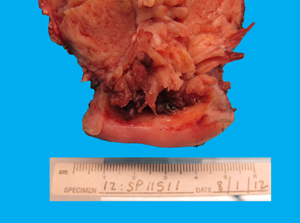
Received was an intact 328 gram specimen consisting of uterus and cervix (11.2 cm from superior to inferior x 6 cm from anterior to posterior x 8.5 cm from right to left), bilateral ovaries and fallopian tubes. The ectocervix was covered by smooth glistening white mucosa with a dilated central cervical os. The endocervical canal had a tan herringbone mucosa. The endometrial cavity (5.5 cm from cornu to cornu x 4.5 cm in length) was completely filled with a soft and friable tan-white polypoid mass (14.5 x 6.8 cm) with finger-like projections (Figure 1). The tumor invaded the myometrium to a depth of 0.5 cm (Figure 2) and extended down to the lower uterine segment without involving the endocervix (Figure 3). The uninvolved myometrium measured 2.7 cm in maximal thickness and was grossly unremarkable. The serosa was smooth. The bilateral fallopian tubes and ovaries were grossly unremarkable.
 |
 |
 |
Microscopic examination:
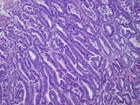
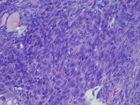
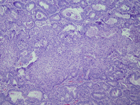
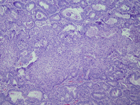
The tumor was biphasic consisting of crowded glands within a malignant mesenchymal component. The glands were lined by atypical proliferative endometrioid-type epithelium (Figure 4). The mesenchymal component consisted of a low-grade sarcoma, resembling an endometrial stromal sarcoma (Figure 5). Metaplastic non-keratinizing squamous epithelium filled the lumen of the glands in several areas (Figure 6). A focus of bone was identified (Figure 7). The pelvic lymph nodes were negative for metastatic carcinoma.
 |
 |
 |
 |

 Meet our Residency Program Director
Meet our Residency Program Director
