Resident Program - Case of the Month
April 2019 - Presented by Dr. Raymond Gong (Mentored by Dr. Dorina Gui)
Diagnosis
C.) Adenomyomatosis, or adenomyomatous hyperplasia, is characterized by cystically dilated glands in the wall of the gallbladder admixed with prominent musculature. When diffuse, adenomyomatosis typically manifests as thickening of the gallbladder wall with a trabecular appearance grossly. As demonstrated by the fundic nodule seen in the current case, adenomyomatosis can often form a pseudotumor, especially in the fundic region. This localized presentation, also referred to as an adenomyoma or adenomyomatous nodule, is more commonly observed than a diffuse pattern.
Adenomyomatosis is not a neoplastic precursor lesion. However, high-grade dysplasia and invasive adenocarcinoma may be associated with these lesions. While there was no evidence of overt dysplasia present in the current case, metaplastic changes of the epithelium were observed. As in other organ systems, metaplasia is a common manifestation of chronic injury in the gallbladder. Cholelithiasis or cholecystitis may lead to metaplasia in up to 75% of cases. As seen in the current case, the most common type of metaplasia is mucinous columnar metaplasia of the gastric type. Known as antral or pyloric metaplasia, this type of metaplasia results in glands morphologically similar to those normally residing in the gastric antrum. Rarer types of metaplasia include intestinal and squamous metaplasia.
Differential Diagnosis
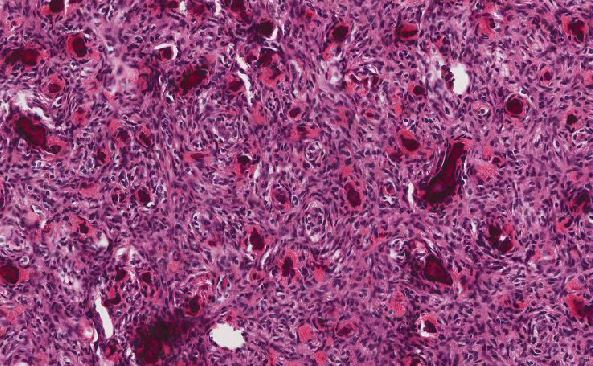
A.) One of the most important considerations in the differential diagnosis is adenocarcinoma, which can be difficult to distinguish from benign processes when there is no preponderance of obvious dysplastic features. Furthermore, mucosal herniations and the intramural proliferation of metaplastic glands, particularly when occurring close to nerves, may be mistaken with adenocarcinoma and perineural invasion. However, characteristic morphologic features can help to identify malignant glands. Architecturally, adenocarcinoma often appears as a densely-packed, random or haphazard arrangement of glands that are usually smaller and irregularly-shaped. While adenomyomatosis often entails the percolation of glands in between muscle bundles, the direct contact of glands with the muscularis favors an invasive adenocarcinoma. Additional helpful features of malignancy include intraluminal necrosis, true perineural invasion, vascular invasion, and the presence of infiltrative single cells or clusters of cells. Cytologically, adenocarcinomas can show nuclear enlargement, nuclear irregularities, hyperchromatism, loss of polarity, and mitotic figures. Nuclear grooves can be helpful in identifying well-differentiated adenocarcinomas. Overall, there was no evidence of the aforementioned malignant features in the current case.
If necessary, immunohistochemistry may be utilized to aid in the diagnosis of adenocarcinoma. Cytoplasmic positivity for the glycoproteins CEA and MUC1 is more common in adenocarcinomas than in benign conditions, especially in high-grade tumors. The overexpression of TP53 and a high Ki-67 labeling index also point to adenocarcinoma.
B.) Fibromyoglandular polyps are benign polyps that are typically small and are believed to represent a regenerative process. Histologically, they are characterized by a localized lesion comprised of fibromuscular stroma containing scattered glands that may show pyloric metaplasia and cystic dilation. Though there may be overlap in morphologic features between fibromyoglandular polyps and adenomyomatosis, the diffuse nature and deeper involvement of the gallbladder wall by the process seen in the current case is more characteristic of adenomyomatosis.
D.) Rarely, mucinous cystic neoplasms arising in the bile ducts and liver can secondarily involve the gallbladder. Similar to the metaplastic pyloric-type glands seen in the current case, the glands of mucinous cystic neoplasms are cystically dilated, can show minimal architectural complexity, and are lined by tall, columnar, mucin-containing cells that can be bland in appearance. However, mucinous cystic neoplasms are typically surrounded by a thick, fibrous capsule and possess septa between cysts that are characterized by a hypercellular stroma resembling that seen in the ovary. Notably, the stromal cells of mucinous cystic neoplasms frequently express estrogen receptor, progesterone receptor, and inhibin. In the gallbladder, adenomyomatosis with hypercellular stroma can be mistaken with true hepatobiliary mucinous cystic neoplasms. The lack of ovarian-type stroma combined with the rarity of hepatobiliary mucinous cystic neoplasms involving the gallbladder make the diagnosis of mucinous cystic neoplasm unlikely in the current case.
References
- Odze RD, Goldblum JR. Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, Expert Consult - Online and Print. Saunders; 2014.
- Albores-saavedra J, Keenportz B, Bejarano PA, Alexander AA, Henson DE. Adenomyomatous hyperplasia of the gallbladder with perineural invasion: revisited. Am J Surg Pathol. 2007;31(10):1598-604.
- Jutras A, Levesque HP, Larini GP. Adenomyoma and adenomyomatosis of the gallbladder. Nunt Radiol. 1964;30:1223-45.
- Beilby JO. Diverticulosis of the gall bladder. The fundal adenoma. Br J Exp Pathol. 1967;48(4):455-61.

 Meet our Residency Program Director
Meet our Residency Program Director