Resident Program - Case of the Month
October 2019 - Presented by Ryan Thomas (Mentored by Kurt Schaberg)
Discussion:
Esophagitis dissecans superficialis (EDS, also called sloughing esophagitis) is a rare benign condition characterized by desquamation, separation and sloughing of the superficial squamous epithelium of the esophagus. The clinical presentation can range from an incidental endoscopic finding to complaints of dysphagia, nausea, and odynophagia. Some presentations can be quite dramatic with regurgitation or vomiting of long segments of sloughed epithelium resembling snake skin.
EDS has been associated with various factors including the use of medications such as bisphosphonates and NSAIDs, autoimmune bullous dermatoses, smoking, drinking hot beverages, and physical trauma such as chemical irritants and medical intervention (e.g., nasogastric intubation, endoscopy, etc.). However, no specific or definite etiology or pathogenesis of this condition has been described, and most cases remain unexplained.
The endoscopic appearance of EDS varies. Mild EDS can appear as fragments of stripped white mucosa without bleeding, linear mucosal breaks, vertical fissures, and circumferential cracks with peeling. More severe cases will appear as a diffuse, thin white membrane that lifts off of the underlying esophageal epithelium, which can show extensive bleeding and exudative esophagitis.
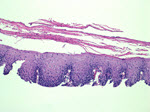
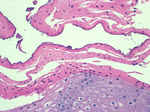
Histologically, EDS is characterized by a cleavage plane near the top of the epithelial layer resulting in a characteristic long, detached fragment of superficial epithelium. Prominent parakeratosis is a typical finding. Fragments of necrotic epithelium without significant inflammation can be present. The basal layer is intact without degeneration or inflammation. Of note, bacterial and fungal colonization can occur, and should not have a significant associated inflammatory response. This represents a potential diagnostic pitfall, as there has been a reported case of EDS that was misdiagnosed as candida esophagitis leading to unnecessary treatment of the patient with antifungal therapy.
Discontinuation of any identifiable precipitating factors in combination with acid suppression has been shown to result in complete resolution of EDS. Prognosis is excellent, with no permanent esophageal injury or other long term-sequelae associated with this condition. It has been proposed that due to a combination of lack of awareness and misdiagnosis, EDS may be more common than its representation in the literature would suggest. More widespread awareness of this condition and its clinical, endoscopic, and histologic features could therefore lead to greater detection and possibly elucidation of its mysterious etiology.
Figure 1: This image shows the characteristic separation of the superficial parakeratotic layer from the underlying epithelium. Note the lack of significant inflammation.
Figure 2: This higher power view highlights the normal underlying squamous epithelium with the prominent superficial sloughing parakeratosis.
References:
- Rawal, K. (2015). "Esophagitis dissecans superficialis". Indian Journal Of Gastroenterology, 34(4), 349-349. doi: 10.1007/s12664-015-0588-x
- De, S., & Williams, G. (2013). "Esophagitis Dissecans Superficialis: A Case Report and Literature Review". Canadian Journal Of Gastroenterology, 27(10), 563-564. doi: 10.1155/2013/923073
- Carmack, S., Vemulapalli, R., Spechler, S., & Genta, R. (2009). "Esophagitis Dissecans Superficialis (“Sloughing esophagitis”)". The American Journal Of Surgical Pathology, 33(12), 1789-1794. doi: 10.1097/pas.0b013e3181b7ce21
- Hokama, A. (2010). "Esophagitis dissecans superficialis and autoimmune bullous dermatoses: A review". World Journal Of Gastrointestinal Endoscopy, 2(7), 252. doi: 10.4253/wjge.v2.i7.252
- Braunberger, T., Hawkes, J., Clarke, J., Boynton, K., & Leiferman, K. (2016). "Esophagitis Dissecans Superficialis Endoscopically Induced in a Patient With Pemphigus Vulgaris and Gastrointestinal Complaints". JAMA Dermatology, 152(8), 948. doi: 10.1001/jamadermatol.2016.1007

 Meet our Residency Program Director
Meet our Residency Program Director
