Resident Program - Case of the Month
July 2021 – Presented by Dr. Alison Chan (Mentored by Dr. Sarah Barnhard)
Discussion
The diagnosis in this case was thrombotic thrombocytopenic purpura (TTP). The patient has fulfilled all five of the pentad criteria for TTP: fever, thrombocytopenia, anemia, renal dysfunction, and neurological symptoms. Additionally, his lab results are consistent with a microangiopathic hemolytic anemia (MAHA): schistocytes and thrombocytopenia on peripheral blood smear, elevated LDH, and decreased haptoglobin. The diagnosis was confirmed with an ADAMTS13 activity test which showed undetectable levels of ADAMTS13 activity.
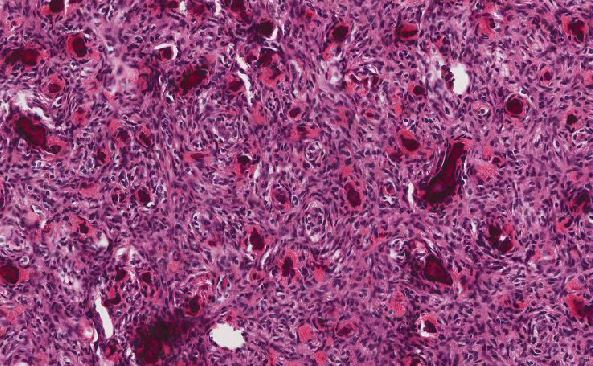
Thrombotic thrombocytopenic purpura is a systemic thrombotic illness that mainly affects the small vessels and is associated with a deficiency of ADAMTS13 enzyme activity. ADAMTS13 is a zinc-containing metalloprotease enzyme that cleaves large von Willebrand factor (vWF) multimers that are anchored in the endothelium. Decreased ADAMTS13 can be due to a congenital mutation in the ADAMTS13 gene, leading to a lack or altered level of enzyme activity, or is more commonly caused by an acquired autoantibody against ADAMTS13 that may inhibit enzyme function or clear the enzyme from circulation (i.e. an ADAMTS13 inhibitor). The exact triggers are unknown, but is thought to be associated with certain diseases, medical procedures, or medications. The decreased ADAMTS13 activity leads to large circulating vWF multimers that lead to microvascular thrombi to form, thus consuming circulating platelets and causing thrombocytopenia. Red blood cells (RBCs) undergo shearing stress as they pass the microthrombi in the small vessels, causing them to rupture and form schistocytes. The free hemoglobin is released from the RBCs which bind to circulating haptoglobin, causing decreased levels of haptoglobin. Lactate dehydrogenase is also released from lysis of RBCs. The direct Coombs test (DAT) as well as the RBC antibody screen will be negative since the hemolytic anemia is not caused by antibodies against RBCs. Additionally, the microvascular thrombi lead to decreased blood flow to organs causing end organ damage, such as renal dysfunction and mental status changes. Clinically, the patients may present with fever, microangiopathic hemolytic anemia, thrombocytopenia, renal impairment, and neurological symptoms. These findings comprise the pentad criteria for TTP, however, all five criteria are not seen in every case.
If there is a suspicion for TTP, physicians can use the PLASMIC score to predict ADAMTS13 deficiency. Patients are scored using this point system which uses criteria such as the platelet count, presence of hemolysis, presence of active cancer, history of solid-organ or stem-cell transplant, MCV, INR, and levels of creatinine. The total points then predict who might benefit from early initiation of therapy due to the likelihood of ADAMTS13 deficiency.
The preferred treatment in the majority of cases is therapeutic plasma exchange (TPE). TPE removes the anti-ADAMTS13 autoantibody and replaces the ADAMTS13 enzyme by using donor plasma as replacement fluid. Common side effects to a plasma exchanges includes allergic reactions to the replacement plasma and hypocalcemia secondary to citrate for anticoagulation. Therapeutic plasma exchanges are typically performed daily until the platelet count is greater than 150 x 109/L and the LDH measures near normal for 2-3 consecutive days. Once this is achieved, the exchanges can be tapered or stopped completely with close monitoring. An alternative treatment involves infusion of donor plasma. Plasma simple transfusions are particularly useful when plasma exchanges are not available or in cases of congenital TTP when native ADAMTS13 is either dysfunctional or physiologically low. Rituximab may be used for cases of refractory or relapsing TTP caused by inhibitors to prevent the production of the ADAMTS13 autoantibody. Rituximab can also be used in adjunct with TPE.
In our case, the ADAMTS13 activity was performed on a STAT basis (same day) using in-house laboratory testing. Most facilities do not have access to same day ADAMTS13 activity testing and thus treatment algorithms recommend starting plasma exchanges empirically while waiting several days for the diagnostic ADAMTS13 activity results from a send out laboratory. TTP is a critical emergency. If left untreated, it is highly fatal with approximately 90% mortality and even with appropriate therapy mortality can approach 20-25%. Thus, there should be a low threshold to treat suspected TTP cases with plasma transfusion or plasma exchange as urgently as possible.
Sources
- Bendapudi PK. Plasmic score for ttp. MD Calc website. Accessed 5/26/2021.
- Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, Pham H, Schneiderman J, Witt V, Wu Y, Zantek ND, Dunbar NM. Guidelines on the use of therapeutic apheresis in clinical practice - evidence-based approach from the writing committee of the American society for apheresis: the eighth special issue. J Clin Apher. 2019;34:171-354. doi: 10.1002/jca.21705
- Smock KJ. The role of adamts13 testing in the work up of suspected thrombotic thrombocytopenic purpura. AACC website. April 1, 2016. Accessed 6/7/2021.
- Thrombotic thrombocytopenic purpura. National Heart, Lung, and Blood Institute website. Accessed 6/7/
- Thrombotic thrombocytopenic purpura. National Organization for Rare Disorders website. Updated 2021. Accessed 6/7/2021.
- Zheng, X Long. “ADAMTS13 and von Willebrand factor in thrombotic thrombocytopenic purpura.” Annual review of medicine vol. 66 (2015): 211-25. doi:10.1146/annurev-med-061813-013241

 Meet our Residency Program Director
Meet our Residency Program Director