Resident Program - Case of the Month
August 2021 – Presented by Dr. Peter Conner (Mentored by Dr. Kristie Vandewalker)
Discussion
Anal adenocarcinomas arise in the glandular epithelium of the anal canal and generally fall under two subtypes: mucosal and extramucosal. Mucosal adenocarcinomas arise in the luminal mucosa, while the extramucosal type arises from an anal gland, pre-existing fistula, or other non-fistulating glandular structure (may be acquired or congenital malformations or embryological remnants).
Anal cancer is uncommon, and it is estimated that anal adenocarcinomas account for about 10% of all anal cancers. Review of reported cases suggests there is a slight male predilection (M:F ratio 1.7:1), with an average age 58 years. Risk factors include smoking, HIV, anoreceptive intercourse, anal Crohn’s disease, and chronic anal fistula. HPV infection has been implicated in a small subset of a tumors (most commonly due to HPV16 or 18).
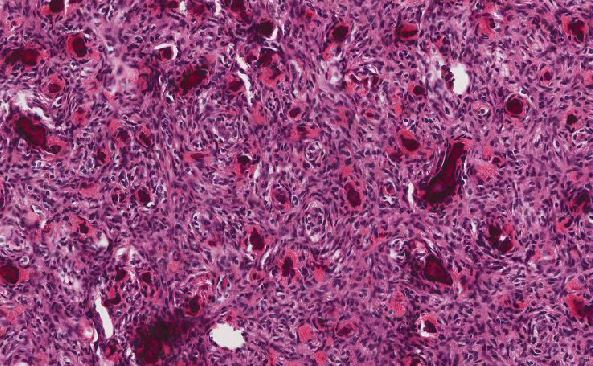
Macroscopically, they often present as mucosal or submucosal lesions and are usually indistinguishable from colorectal adenocarcinoma. Microscopically, mucosal type anal adenocarcinomas have histologic features of indistinguishable from rectal adenocarcinoma (such as intestinal type morphology). All types of anal adenocarcinoma may show pagetoid spread of anal squamous mucosa or perianal skin (secondary anal Paget disease). The secondary Paget cells may be contiguous with the underlying neoplasm or far away (skip lesions), and in some cases, present months to years before or after the underlying adenocarcinoma becomes detectable. These tumors tend to be positive for CK20 and CDX2 and can be positive or negative for CK7.
Primary anal Paget disease is believed to arise from perianal skin and can extend into the anal canal mucosa, become invasive, and mimic primary anal canal adenocarcinoma. These tumors typically coexpress CK7 and GCDFP-15 and are negative for CK20 and CDX2.
There is limited data on the molecular pathology of anal canal adenocarcinoma; however, there appears to be some association with KRAS and NRAS mutations and rare observation of microsatellite instability.
The prognosis of these tumors are generally worse than their squamous cell counterparts; however, it is largely dependent on staging.
References
- Gonzalez RS. Paget disease. PathologyOutlines.com website. Accessed July 19th, 2021.
- Marti L, Nussbaumer P, Breitbach T, Hollinger A. Das perianale mucinöse Adenocarcinom. Ein weiterer Grund für die histologische Untersuchung bei Analfistel oder Anorectalabscess [Perianal mucinous adenocarcinoma. A further reason for histological study of anal fistula or anorectal abscess]. Chirurg. 2001 May;72(5):573-7. German. doi: 10.1007/s001040170137. PMID: 11383070.
- Schaffzin DM, Stahl TJ, Smith LE. Perianal mucinous adenocarcinoma: unusual case presentations and review of the literature. Am Surg. 2003 Feb;69(2):166-9. PMID: 12641361.
- WHO Classification of Tumours Editorial Board. Digestive system tumours. Lyon (France): Internation Agency for Research on Cancer; 2019. (WHO classification of tumours series, 5th; vol. 1).

 Meet our Residency Program Director
Meet our Residency Program Director