Resident Program - Case of the Month
May 2023 – Presented by Dr. Melissa Ha (Mentored by Dr. Ananya Datta Mitra)
Discussion
Classic Hodgkin lymphoma (CHL) is a neoplasm of germinal B-cell lineage that primarily affects lymph nodes, although extra-nodal sites like spleen, lung, and bone marrow may also be involved. Neoplastic cells can be multi-nucleated with a distinct “owl-eyes” appearance known as Reed-Sternberg cells or appear mononuclear and atypical called Hodgkin cells. The background is usually composed of a varying mixture of reactive inflammatory cells including small mature lymphocytes, histiocytes, neutrophils, eosinophils, and plasma cells. Based on the background nonneoplastic immune infiltrate and other differences in morphology, four subtypes of CHL have been classified by the World Health Organization. The subtypes are nodular sclerosis, mixed cellularity, lymphocyte rich, or lymphocyte deplete.
CHL and all its subtypes account for approximately 90% of Hodgkin lymphomas. As a whole, the subtypes display a bimodal age distribution with the highest incidence in individuals 15-35 years of age and a second peak affecting individuals 50-70 years old. However, more specific epidemiology profiles vary by subtype.
The etiology is incompletely understood, but there are associated risk factors that predispose to CHL including HIV infection, EBV, and prior mononucleosis. It is postulated that in an immunocompromised state, viruses can drive tumorigenesis, allowing neoplastic Hodgkin and Reed-Sternberg (HRS) cells to evade immunosurveillance. Thus, in situ hybridization for EBV encoded RNA studies for suspected cases of CHL is warranted. Among the four subtypes, mixed cellularity is most commonly associated with EBV (approximately 70% of cases).
Classic Hodgkin lymphoma is characterized by the paucity of HRS cells. Such scant population of fragile malignant cells are not typically detectable by flow cytometric analysis. Therefore, a negative flow result should not exclude Hodgkin lymphoma (HL). Conversely, flow cytometry often reflects the background reactive infiltrate, so the presence of a mixed population of immune cells should raise concern for HL.
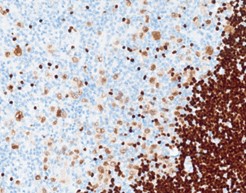
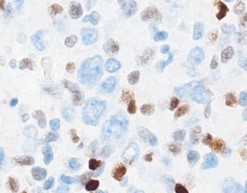
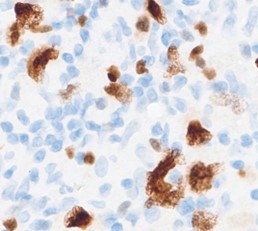
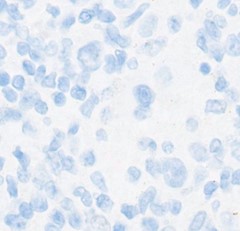
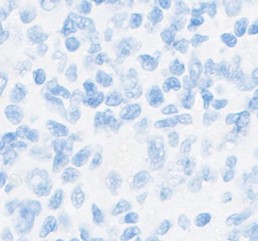
Unlike the malignant counterparts of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), Hodgkin and Reed-Sternberg (HRS) cells of CHL are characterized by loss of most B-cell antigens showing negative or diminished staining for CD20, CD79a, OCT2, BOB1 and dim/blush PAX5. They also show loss of CD45, a hematopoietic cell marker, but display a characteristic perinuclear Golgi dot-like staining pattern for CD15 and CD30. MUM-1 may be retained as evidence of B-cell lineage.
On the other hand, the malignant cells of NLPHL (answer choice A) generally retain B-cell phenotype and express CD20, OCT2, CD75, CD79a, BOB1, PAX5, and CD45. In almost all cases, they lack CD15 and CD30.
Neoplastic component of DLBCL (answer choice B) consists of large, atypical cells that may have RS-like morphology, especially EBV+ DLBCL. However, malignant cells typically stain positive for B-cell markers including CD19, CD20, CD79a, and PAX5. Although CD30 is variably expressed, CD15 shows negative staining.
Anaplastic large cell lymphoma (answer choice C) is a peripheral T-cell lymphoma comprising of large atypical lymphoid cells called Hallmark cells. These cells are characterized by ALK positivity on immunohistochemical stains. CD30 staining may also display perinuclear dot like pattern, but CD15 is typically negative. B-cell markers including PAX5 and CD20 stain negative and T-cell markers (CD2, CD4, CD5) stain positive to help distinguish from CHL.
Plasmablastic lymphoma (answer choice E) is derived from a post-germinal plasmablast showing large immunoblast morphologic features and has high association with HIV and EBV. However, flow cytometry would demonstrate a monoclonal population with plasma cell markers (CD138 and CD38) and light-chain restriction.
Other immunohistochemical stains supporting CHL diagnosis is included below:
References
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, eds. "WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues 2017 (Revised 4th ed.)". International Agency for Research on Cancer; 2017.
- "Title: Non-B cell lymphomas - classic type". PathologyOutlines.com website. Accessed April 25, 2023.

 Meet our Residency Program Director
Meet our Residency Program Director
