‘That I was able to recover gives them hope’: Respiratory therapist shares COVID-19 experience
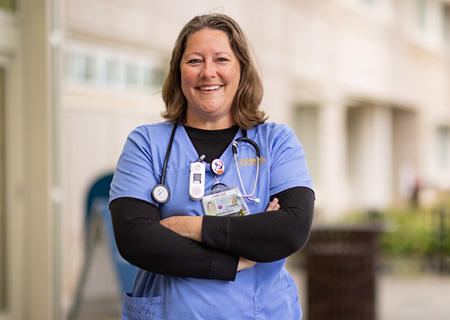
When the COVID-19 pandemic hit the United States in March 2020, Chelsie Gilbeau, who specializes in respiratory care, stepped to the front lines to care for some of the most critically ill patients at UC Davis Medical Center.
As a respiratory therapist, Gilbeau’s role was to help patients with their breathing or airway problems. One condition she treated was acute respiratory distress syndrome, a serious condition that can occur with COVID-19.
“I still remember how much sicker our COVID-19 patients were than our other patients,” Gilbeau said. “Most of our usual treatments for other respiratory diseases did not work for our COVID-19 patients. Ventilators usually helped, but proning (placing a person facedown) patients did not alleviate their symptoms.”
Health care provider becomes a patient
After a few weeks of working in the hospital with COVID-19 patients, Gilbeau came down with what she first thought was a cold. Soon her symptoms worsened, and she tested positive for COVID-19. Still, she thought she could take care of herself at home.
“I did everything I could to not go to the hospital,” Gilbeau recalled. “I was really sick, but as an experienced specialist in respiratory care, I knew how to manage my symptoms and give myself breathing treatments if needed.”
Within days, Gilbeau’s most intense COVID-19 symptoms abated, but she was still struggling with a lingering cough and dizziness. Her heart rate would jump to 170 just from getting up to go to the bathroom.
After speaking with her primary care physician, Gilbeau was referred to Richart Harper, interim division chief of Pulmonary, Critical Care and Sleep Medicine at UC Davis Health. She was soon diagnosed with Postural Orthostatic Tachycardia Syndrome (POTS) – an abnormal increase in heart rate that occurs after sitting up or standing. She was later also diagnosed with post-COVID, sometimes also called long COVID.
The symptoms of POTS include but are not limited to:
- lightheadedness (occasionally with fainting)
- difficulty thinking and concentrating (brain fog)
- fatigue
- intolerance of exercise
- headache
- blurry vision
- palpitations
- tremors
- nausea
“It was definitely a scary diagnosis, but I was happy to finally know what I was dealing with,” said Gilbeau.
Rehabbing from post-COVID
To treat her condition, Gilbeau was referred to UC Davis Health's Pulmonary Rehabilitation Program. The program has been supporting patients with post-COVID symptoms since early in the pandemic.
The Pulmonary Rehabilitation Program at UC Davis Health is accredited by the American Association of Cardiovascular and Pulmonary Rehabilitation. It empowers patients with lung conditions through education, exercise, motivation and support to help improve their quality of life. The multidisciplinary team of specialists provide a wide range of care including a comprehensive evaluation, monitored and supervised exercise, education, psychosocial support and nutritional guidance.
Exercises and therapies with post-COVID patients include seated exercises with Therabands, weights, cardio and practicing proper breathing techniques. Throughout the exercises, respiratory therapists continuously monitor patient’s heart rates, oxygen levels and blood pressure.
“Pulmonary rehab was super helpful – it helped me learn how to do things in moderation and not exacerbate my symptoms,” said Gilbeau. “I still am dealing with occasional trouble breathing and dizziness, but it is now much more manageable.”
Giving hope to others
After five months of treatment and rehab, Gilbeau returned to UC Davis Medical Center to resume caring for COVID-19 patients.
While treatment options for COVID-19 patients have improved since the beginning of the pandemic, Gilbeau notes that COVID-19 patients are still scared when they are hospitalized.
“A lot of our hospitalized COVID-19 patients still think they are going to die,” shared Gilbeau. “To be able to share with them what I went through and show them that I was able to recover gives them hope. I am happy to be able to not just care for them physically while they are sick, but also be able to inspire them in their recovery.”
Related stories
- Lessons from the long-COVID clinic
- What to know about long COVID from doctors who’ve treated it (Capital Public Radio)
- Learn more about UC Davis Health’s Long COVID clinic
- Learn more about coronavirus, including vaccines, treatments and more at UC Davis Health




