Do microRNAs hold the key to psychiatric and neurodegenerative disorders?
Study identifies specific microRNAs in the brain that likely contribute to bipolar disorder, depression, schizophrenia, PTSD and Parkinson’s disease
A study in Nature Aging from researchers at the UC Davis School of Medicine has identified specific microRNAs — non-coding RNAs that regulate gene expression within cells — that likely contribute to bipolar disorder, depression, schizophrenia, post-traumatic stress disorder (PTSD) and Parkinson’s disease.
“To our knowledge, this is the first study to identify microRNAs that contribute to the development of psychiatric and neurodegenerative diseases,” said Aliza Wingo, senior author of the study. Wingo is a professor in the UC Davis Department of Psychiatry and Behavioral Sciences and a staff psychiatrist at VA Northern California Health Care.
MicroRNAs act like brakes
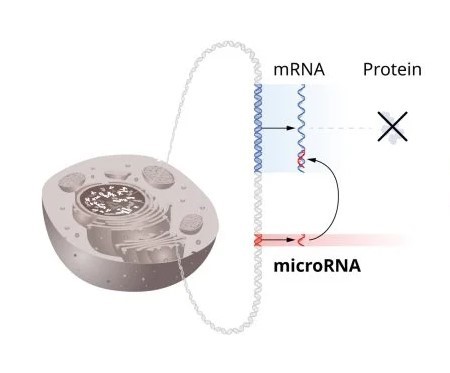
Genetic instructions for living organisms are contained within the DNA in a cell’s nucleus.
Messenger RNA (mRNA) is responsible for carrying protein-making instructions from the DNA in the cell’s nucleus to the cytoplasm, the gelatinous liquid that fills the cell.
In the cytoplasm, the mRNA instructs the cell’s protein-making machinery — organelles like ribosomes — to make specific proteins based on the instructions received from the DNA.
But a different and very small type of RNA, microRNAs, can put the brakes on this protein-making process.
First discovered in 1993, microRNAs can stick to mRNA and prevent the protein encoded on it from being made.
As a braking mechanism, microRNA regulates the cell, making sure it develops normally. But research shows abnormal regulation from microRNA can contribute to health disorders.
More than 2,000 microRNAs have been discovered in humans. Abnormal regulation from microRNAs — and how it may contribute to a wide range of diseases — has become a new area of focus for researchers.
Study methods
The study used post-mortem brain samples from 604 donors (432 female and 172 male) recruited by the Religious Orders Study/Rush Memory and Aging Project. The longitudinal study was launched in 1994. The participants were older, over 70 at the time of death, with a median age of death of 90 years.
The researchers looked at tissue from the dorsolateral prefrontal cortex, a region toward the front of the brain involved in cognitive processes, working memory and planning.
From the samples, the researchers identified genetic variants associated with brain microRNA levels.
Then, they combined this information with results from genome-wide association study (GWAS) data for 16 psychiatric and neurodegenerative diseases.
“To our knowledge, this is the first study to identify microRNAs that contribute to the development of psychiatric and neurodegenerative diseases.”—Aliza Wingo, professor, Department of Psychiatry and Behavioral Sciences
Findings
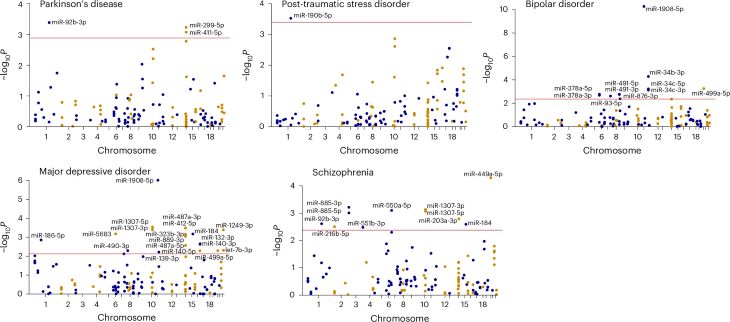
The researchers identified 49 unique microRNAs associated with one or more brain traits, including major depression, PTSD, bipolar disorder, schizophrenia and Parkinson's disease.
Performing further analyses, they identified four unique microRNAs that likely contribute to the development of the following psychiatric and neurodegenerative diseases:
- miR-499a-5p: bipolar disorder and schizophrenia
- miR-92b-3p: Parkinson’s disease
- miR-190b-5p: PTSD
- miR-1908-5p: bipolar disorder and major depressive disorder
"Interestingly, miR-499a-5p contributes to the risk of both bipolar disorder and schizophrenia, and miR-1908-5p to the risk of both bipolar disorder and major depression,” said Wingo. “These findings suggest potential shared mechanisms between these pairs of conditions through microRNAs."
The researchers also looked at microRNA expression quantitative trait loci (miR-QTLs). These are genetic variants that can influence the levels of microRNAs.
Nearly half (224 of 470) of the analyzed microRNAs were shown to have associated miR-QTLs, pointing to potential genetic factors influencing microRNA.
Limitations
The authors note several limitations of the study. All the subjects were older adults of European ancestry. Subsequent studies that include people of diverse ancestry and a wider age range may offer more insights. Another limitation is that the study focused only on one specific brain region — the dorsolateral prefrontal cortex — and may not be typical of other brain regions.
Understanding contributors to disease
“We know microRNAs regulate gene expression, with a single microRNA potentially influencing hundreds of genes,” said Thomas Wingo, co-senior author of the study. Wingo is a professor in the UC Davis Department of Neurology and specializes in treating patients with mild cognitive impairment and dementia. “Our findings advance understanding of how microRNAs contribute to the risk of major psychiatric disorders and Parkinson's disease.”
Additional authors include Selina M. Vattathil, Ekaterina S. Gerasimov and Yue Liu of UC Davis School of Medicine; Se Min Canon, Paul J. Kim, Adriana Lori and Sarah Sze Min Tan of Emory University School of Medicine; Eric C. Lai of Sloan Kettering Institute; and David A. Bennett of Rush University Medical Center.