Innovative procedure buys time for newborn who needs heart surgery
Carter Vincent is living proof that a unique approach by doctors at UC Davis Children’s Hospital could successfully stave off major cardiac surgery just days after his birth.
Carter was born with a single ventricle defect in his heart, which caused too much blood flow to his lungs and risked inadequate blood flow to his body.
At any other hospital, his surgical path might have gone the way of decades of congenital heart patients before him. At only a couple of days old, he would have received the Norwood procedure, his first open-heart surgery in a three-stage procedure to rebuild his heart and restore proper circulation of oxygen-rich blood to his body.
But instead, the UC Davis Children’s Hospital team innovated to buy some time for this newborn to adjust to post-fetal life, grow and develop more, before moving forward with an open-heart surgery.
“We wanted to try rerouting his blood flow so he could go home and adjust to the world in his first days of life instead of recovering from open-heart surgery,” said Frank Ing, interventional cardiologist, chief of pediatric cardiology and co-director of the UC Davis Pediatric Heart Center. “I am not sure any other center on the West Coast is doing this.”
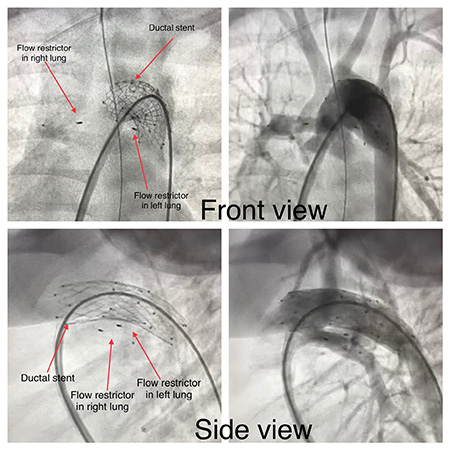
Ing describes the procedure as a hybrid Norwood without the hybrid, which involves implanting a stent in the ductus to secure oxygenated blood flow to the body and implanting flow restrictors in the pulmonary arteries to prevent too much blood into the lungs.
This procedure is traditionally performed by open-heart surgery as the first-stage Norwood operation, typical for the single-ventricle patient.
The procedure would enable the team to postpone his heart surgery by eight weeks, allowing Carter to gain weight, learn to eat, give his organs more time to develop and reduce any potential risks that come with cardiac surgery so soon after birth.
“When we first heard that Carter needed surgery and that Dr. Ing had a new technique that would allow us to postpone the surgery, we were on board,” said Elizabeth Vincent. She and her wife Christine are Carter’s parents, and both work in the medical field. “I knew there was a 75-80% survival rate of babies with this surgery soon after birth and we were happy to postpone, if that was an option.”
We wanted to try rerouting his blood flow so he could go home and adjust to the world in his first days of life instead of recovering from open-heart surgery. I don’t think anyone on the West Coast is doing this.” —Frank Ing
Cath procedure proves successful
During the cath procedure, the cath team implanted bilateral flow restrictors in Carter’s pulmonary arteries and performed a ductal stent. They were able to do everything in the cath lab, to help secure and balance the baby’s systemic and pulmonary blood flow. The final saturation was 80 to 85%, which is the ideal number after a surgical Norwood operation.
The minimally invasive procedure was performed completely in the catheterization (cath) lab without making any surgical incisions in the operating room. By the evening of the procedure, Carter had already recovered and was back to his baseline.
“Everything went remarkably well. Carter has gained all the weight that he needed to, and his oxygen levels are where they need to be,” said Elizabeth Vincent, noting that Carter had no big scars and no lengthy surgeries to recover from at such a young age. “We’re so lucky that Dr. Ing was available to do these procedures.”
Pediatric cardiothoracic surgeon Gary Raff followed up with the first surgery of the Norwood procedure when Carter was 8 weeks old. The surgery was a success and Carter recovered in the state-of-the-art UC Davis Pediatric and Cardiac Intensive Care Unit. He is now back at home.
“I’m hopeful that we can provide these types of cath procedures to more babies born with congenital heart defects,” Ing said. “Carter is living proof of how well this can work.”





