Simulated reality provides critical training for School of Nursing students
65-year-old Julia Morales always believed in following your dreams and being true to yourself. She was shattered to learn she had lung cancer four years ago.
But after fighting the good fight, she decided to stop treatment and “just let go.”
Morales lost her fight, in the arms of her partner Lucy Gray, and in the presence of nursing graduate students at the Betty Irene Moore School of Nursing at UC Davis.
Morales and Gray are fictional, yet very lifelike characters. And the future nurses caring for them in this end-of-life experience are part of a loosely scripted and well-choreographed simulation exercise.
“It’s very rare that students experience a patient death in their clinical rotations, because oftentimes, when a patient is about to die, the students move to the background or out of the area altogether,” explained Terri Harvath, professor in the Master’s Entry Program in Nursing (MEPN) and actor in these simulations. “For most of us who are nurses and nursing faculty, our first patient death was when we were out in practice.”
Authentic surroundings promote genuine learning
Ellen Jones is a 79-year-old retired schoolteacher who was recently discharged home with an IV line for antibiotics following hospitalization for cellulitis. When her daughter Cindy visits, she notices that her mother is becoming more forgetful and is not following COVID-19 precautions. She shares those concerns with the home health nurses — in this case, nursing students in the one-bedroom apartment simulation suite in Betty Irene Moore Hall.
“Simulation is best when it is as authentic to the real experience as possible,” Harvath said. “The physical environment in which we do that aids tremendously.”
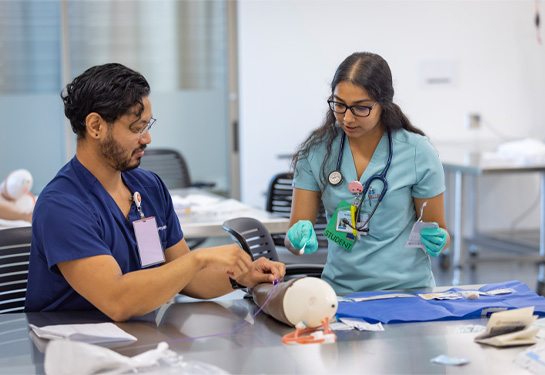
Not only is the environment authentic, so are the actors playing the roles. The School of Nursing team behind the simulations don hair, makeup and attire, along with assuming the voice, mannerisms and physicality of the patients they are playing. Scenes are intentionally loosely scripted so that they are more dynamic. Faculty know certain points they need to include, but they leave plenty of room to adapt based on student reaction in real time.
In the Jones scenario, students are thrust into a tumultuous family dynamic. An older woman with increasing dementia is arguing with her daughter whom she believes wants to put her in a memory care unit. The daughter, over the period of three years, shows burnout as her mother’s caregiver. The students’ assessments of cognitive decline and possible depression serve as screenings for diagnosable medical conditions. They must also identify what community resources are available to the family and how family dynamics play a crucial role in someone’s health and well-being.

Nervous encounters lead to learning experiences
The Julia Morales simulation begins in the hospital ward simulation with an actor playing the role of Julia. It concludes in the bedroom of the apartment simulation with a high-fidelity manikin, which Harvath can program to die.
Students, in pairs, play the role of the nurse. They must make home visits to help manage Julia’s pain, which raises questions about giving opioid analgesics to someone with diminished respirations. Ultimately, they are the ones who, after checking for the absence of heart activity, must inform Lucy that her partner has passed.
“I had a lot of nerves going in. I wanted to be someone who could provide a therapeutic space for a person going through a difficult time,” explained second-year graduate-nursing student Emily Boone. “I went all in and was completely immersed. There’s a reason I want to be a nurse, but after this experience, I’m more sure of my purpose. I know how to be present and helpful, without being overwhelmed by emotion. I feel much better prepared when that moment inevitably comes.”
Familiar circumstances foster improved communications
Boone says the simulation was so real that she completely forgot that faculty were playing a part.
The patient and family member roles are typically played by paid actors who follow a detailed script. In light of COVID-19 restrictions the past two summers, School of Nursing faculty and staff assumed the roles of the various characters in each scene. Megan Hansen, a communications specialist in the UC Davis Health simulation center, acted as Lucy, Julia’s partner. For her, the end-of-life experience felt eerily familiar.
“Having been in a similar position with my grandmother, the tears easily flowed. I was so impressed by how the nursing students handled me and the situation. Emily immediately asked if she could hold my hand,” Hansen recalled. “These are the types of caring, emotionally intelligent and amazing nurses that we need in the world. I would entrust them with my care and the care of my loved ones in a heartbeat.”
These two simulations come in the fifth of the six-quarter program, when students take both the Fostering Healthy Communities and Nursing Care of Older Adults courses. At this point, nursing students have enough clinical experience under their belt to bring that knowledge and experience to a complex set of scenarios.
Harvath knows how emotional these simulations are for all involved. With the mental and physical toll that the pandemic has taken, these cases also hit close to home for many students. While robust learning happens during the half-hour experiences, the takeaways are even richer because of the hour-long debriefings that occur afterwards.

“Some students get quite emotional in the debrief, which allows us to have a conversation about how your humanity in nursing is so important,” Harvath explained. “We don’t want them to wall off emotions, but rather develop the muscle to control it so a family doesn’t have to support the nurse who is distraught.”
“All of us were nervous, because we wanted to do well and not make a gaffe or say the wrong things,” said nursing student Quinn Dai La. “Ideally, we’ll pull these experiences and skills we’ve gained from these simulations and apply them to real life.”
While these two simulations are not enough to cultivate expertise in these areas, faculty say they successfully expose students to sensitive issues. They also provide them with resources and some language to draw on in the future when the experiences — and the patients — are real.
“It is incredibly rewarding, and it makes me feel the work we do and all the hours we spend on these simulations is worth it,” Harvath said. “It allows the students to synthesize and pull it all together.”