The state of California's caregivers

Scaling services to support California's caregivers
UC Davis nursing school report indicates increase in complex care leads to decline in mental and physical health
About one in five Americans provides care to a family member. The complexity and intensity of caregiving for older adults and people with disabilities is increasing, as the population ages and more individuals are living longer with physical, cognitive and mental health challenges.
For caregivers in California who tap into a statewide network of support organizations, the care they provide is more complex than the general population of caregivers. And they are at higher risk of mental and physical health decline.
Those are findings from a new report from the Family Caregiving Institute at the Betty Irene Moore School of Nursing at UC Davis working in conjunction with the Family Caregiver Alliance and California Caregiver Resource Centers.
“Our evaluation shows that these resource centers serve clients at a higher risk when compared to the general population of caregivers,” said Janice F. Bell, associate dean for research at the School of Nursing and co-principal investigator. “They are engaged in more intense care, longer hours and increased responsibilities. They also report more adverse physical and mental health effects from their caregiving role, including isolation and loneliness.”

In 2019 — well before the pandemic — the California Department of Health Care Services invested $30 million in a project, “Picking Up the Pace of Change: Scaling Services for a Changing Caregiver Profile,” to expand and improve family caregiver services from the 11 California Caregiver Resource Centers (CRC) across the state.
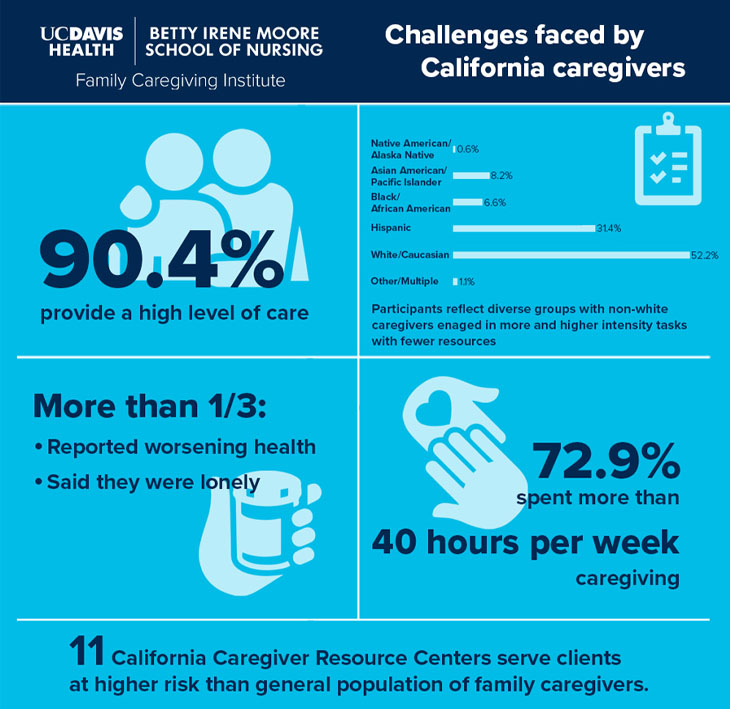
During the second year of the project, the data showed that 90% of those surveyed were providing complex and intense care. Other notable findings of those surveyed include:
- 72.9% spent more than 40 hours per week providing care
- 35% reported worsening health over the past year
- 35% were lonely
“This study is one of the first in the nation that we're aware of with this size and this diversity, consistent with the diversity of California along many dimensions. It’s humbling to see the findings of the intensity of care in our sample,” explained Heather M. Young, co-principal investigator and institute associate director for strategic partnerships. “In general, Black, Hispanic and Native American caregivers spend more time providing care with fewer resources.”
The study gathered information to help the CRCs prioritize outreach and service for those most in need. Over the past year, the project team deployed an interactive platform, CareNav™ to promote uniform quality and availability of core services statewide. CareNav™ includes a caregiver assessment, a record of CRC services provided, consumer information, and the capacity to develop individualized care plans and tailored resources, securely.
“While challenging to deploy the online platform during a pandemic, we found it was a program that really met the needs and enabled many caregivers to get support and services they would not have been able to access with social distancing,” Young added.
"To have someone see me and say, ‘Hey there's actually help for you too,' I thought, 'Wow, I've got to check this place out,' said Simone Nazzal, a CRC client. “I was really pleased to be connected with a family consultant who plugged me into the exact services that I needed in that moment to maintain my sanity and to continue doing this for my mom.”
The research team next hopes to look at the risk profile of the caregivers that are served by the CRCs and examine whether they can identify risk factors for poor outcomes and intervene more quickly.
In the coming year, with funding from Archstone Foundation, the team will also examine ways to identify and better support caregivers engaged in the most complex care and at highest risk for poor health outcomes. Rounding out the investigative team are Jennifer Mongoven, Tina Kilaberia, Benjamin Link and Robin Whitney.

