Residency Program - Case of the Month
August 2016 - Presented by Nicholas Coley, Mirna Lechpammer and Mingyi Chen
Clinical History
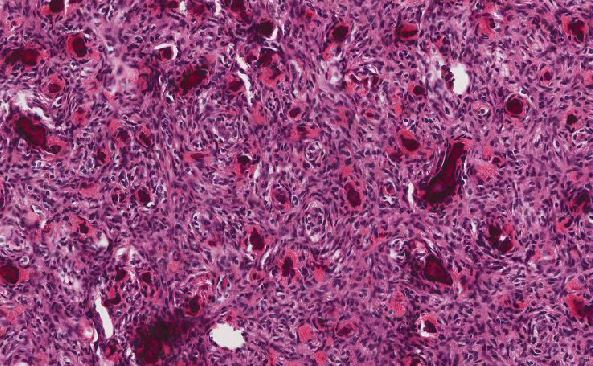
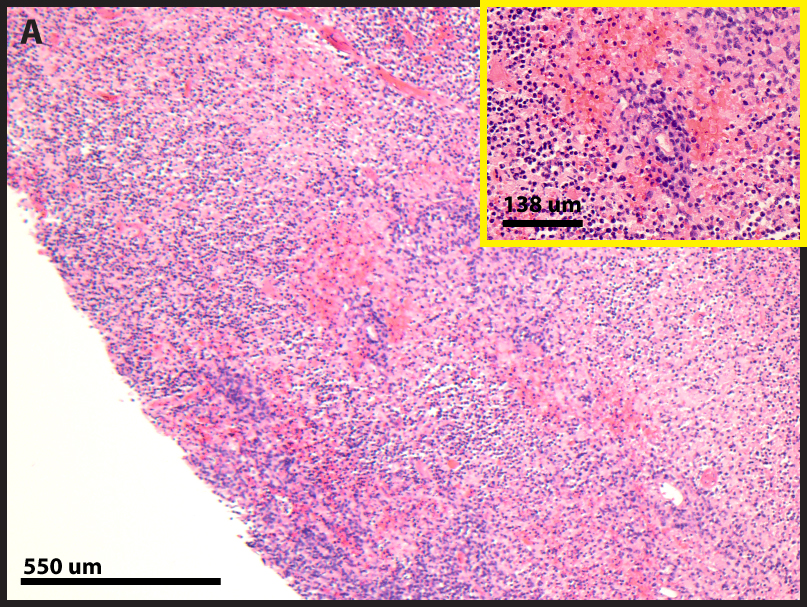
The patient is a young adult with a history of systemic lupus erythematosus (SLE) complicated by class IV-V lupus nephritis requiring prolonged immunosuppression on a multi-drug regimen. New onset headaches, confusion, and behavioral changes prompted evaluation by neurology. The patient experienced a new onset seizure during an initial attempt at central nervous system (CNS) imaging. Subsequent successful imaging demonstrated a large 6.5 cm necrotic mass with extensive edema occupying the left parietal lobe and extending into the cerebellar vermis. Biopsy of the lesion demonstrated extensive tissue necrosis punctuated by rare foci of viable tumor cells (Figure 1). The tumor cells intimately associated with the cerebral vasculature demonstrated positivity for CD20 and PAX5 (Figure 2). A portion of the specimen was submitted for flow cytometry analysis, but the results were indeterminate due to poor cellular viability.
Click on image to enlarge.
| Figure 1A | Figure 1B | |
 |
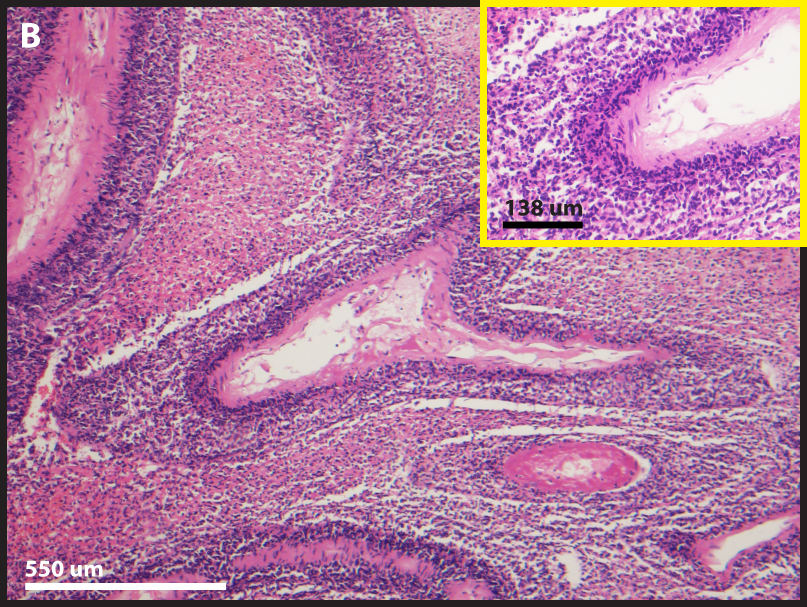 |
Figure 1 A, B. Tumor cells are closely associated with vasculature in a background of extensive necrosis.
| Figure 2A | Figure 2B | |
 |
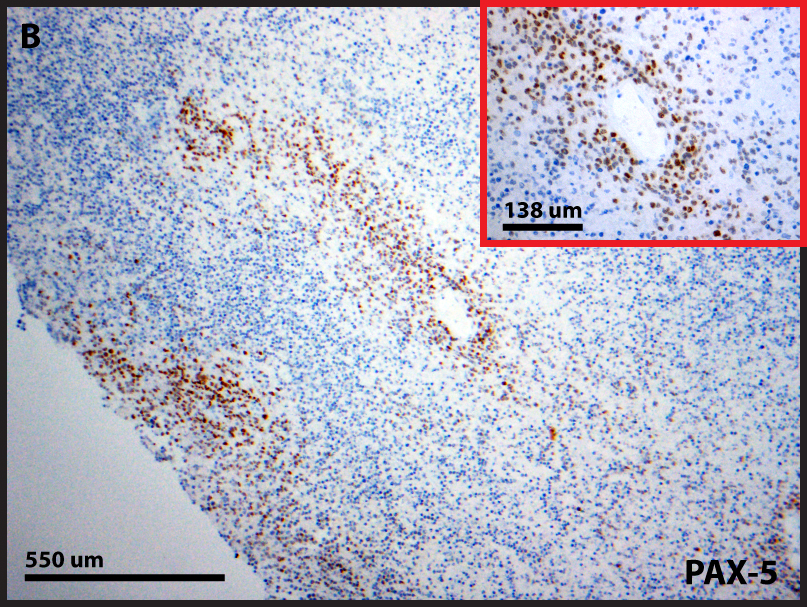 |
Figure 2A. Tumor cells express the B cell antigen CD20.
Figure 2B. Tumor cells express the B cell master transcription factor PAX5.
What is the diagnosis?
Choose one answer and submit.
C. Immunosuppression-related B cell Lymphoproliferative Disorder of the CNS
> Learn more about this diagnosis.

 Meet our Residency Program Director
Meet our Residency Program Director