Resident Program - Case of the Month
November 2018 - Presented by Andrew D. Jones (Mentored by Kristin Olson)
Background
A 34-year-old woman presented to our institution with a history of acute abdominal pain, nausea, and non-bilious, non-bloody vomiting. She had a history of lupus nephritis for which she was treated with peritoneal dialysis as an outpatient. She was found to have a polymicrobial bacterial peritonitis and positive blood cultures, with negative CT and vaginal ultrasound scans. She was treated with antibiotics and her peritoneal catheter was removed. Her abdominal pain diminished and her white cell count decreased.
She then developed acute right lower quadrant abdominal pain and leukocytosis. Her pain increased and became refractory to narcotics, and a third CT a week later showed intraperitoneal free air and thickening of the ascending and descending colon. Exploratory surgery revealed a gangrenous perforated appendix with diffuse peritonitis and a pelvic floor abscess. Her appendix was removed, and her recovery was complicated by additional intraperitoneal fluid collections (requiring IR drainage), fluid overload (requiring an ICU stay), and C. difficile colitis.
Findings
Grossly, her appendix was gangrenous and perforated with marked fibrinopurulent exudate (see Figure 1). The lumen was distended and filled with a granular brown material. Histologic sections revealed innumerable crystalline bodies within the appendiceal lumen and invested within the inflamed epithelium (see Figures 2, 3, and 4). The crystals show a characteristic shape with curvilinear intersecting lines and two-tone coloration.
Click on image to enlarge.
Figure 1: Gross appearance of the cut surgace of the appendix, with fibrinopurulent exudate and granular brown luminar contents.
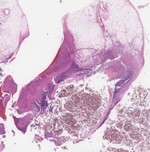
Figure 2: A low power view of the midportion of the appendix. There is significant acute appendicitis and peri-appendicitis. The lumen of the appendix is filled with pink to brown crystals.
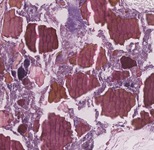
Figure 3: The crystals are pink-orange in color on high power and have characteristic fracture lines that intersect at curved points, imparting a "fish scale" appearance.
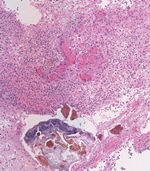
Figure 4: Crystals are intimately associated with prominent granulation tissue on high power. Crystals in areas of granulation tissue and bacterial overgrowth have a more brown-tinged hue.
Which of the following pharmacologic agents is most compatible with the findings shown in the gross and microscopic photos?
Choose one answer and submit.


 Meet our Residency Program Director
Meet our Residency Program Director
