March 2021 – Presented by Dr. Jiejun Wu (Mentored by Dr. John Paul Graff)
The patient is a 49-year-old male with a history of untreated HIV complicated by previous pneumocystis jiroveci pneumonia, recent histoplasmosis and blastomycosis, CMV infection, oropharyngeal candidiasis, syphilis, and delusional disorder. He presents with RLQ abdominal pain and is found to have right external iliac vein thrombosis in the setting of new retroperitoneal and mesenteric lymphadenopathy. The involved lymph nodes are biopsied for pathological evaluation and the clinical team are concerned with “advanced HIV and new lymphadenopathy suspicious for malignancy”.
The received core biopsies show focal necrosis, lymphocytes, plasma cells, and poorly formed granulomata (Figure 1) and the results of flow cytometry are nonspecific because of limited specimen. Since the incidences of both non-Hodgkin (60-200 times) and Hodgkin (5-20 times) lymphomas are prevalent in HIV positive patients, IHC staining is performed to address this concern (Figure 2A-F). In addition, negative or rare staining is found with c-MYC, BCL-1, BCL-6, CD10 and CD30. GMS-F and PAS staining are also tested with this specimen (Figure 3A-B).
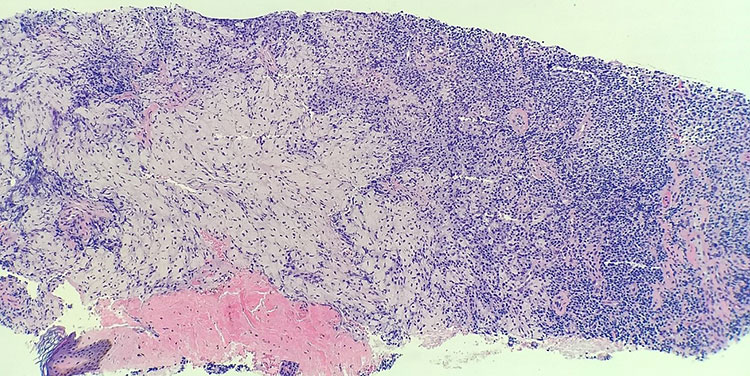
Figure 1 Core biopsy from retroperitoneal lymph nodes. H&E, 100x.
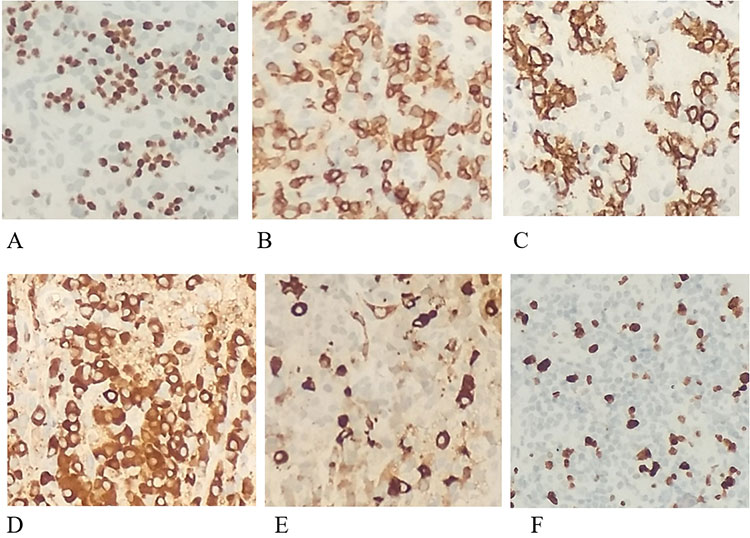
Figure 2 IHC, 400x. A PAX5. B CD3. C CD138. D Kappa. E Lambda. F Ki67.
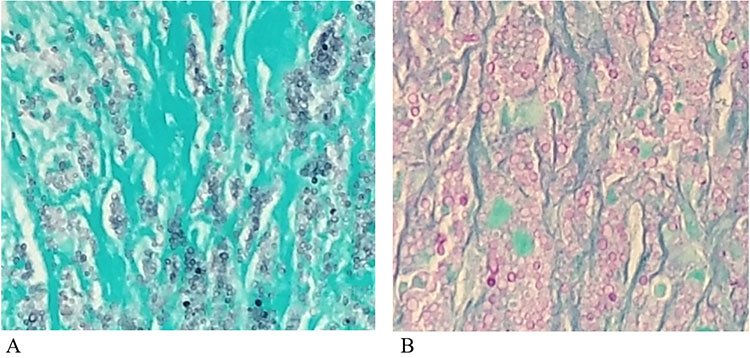
Figure 3 Special staining, 400x. A GMS-F. B PAS.

 Meet our Residency Program Director
Meet our Residency Program Director
