April 2022 – Presented by Dr. Ahresh R. Saha (Mentored by Dr. Elham Vali Betts)
An 18-year-old female presented to the Emergency Department (ED) in May of 2020 after the patient's friend noticed she had a lump on her neck. The patient was told she had swollen lymph nodes. She denied any fevers, chills, night sweats, weight loss, dyspnea, dysphagia, odynophagia, cough, shortness of breath, abdominal pain, or other symptoms. She was given prednisone to decrease inflammation, which she took for 6 days without any improvement in her symptoms. Five months after the initial presentation she presented again to the ED as she noticed the right sided neck mass was growing. CT scan of the neck and chest showed extensive right cervical lymphadenopathy concerning for malignancy, partially visualized soft tissue density in the anterior mediastinum, enlarged right supraclavicular and posterior cervical lymph nodes, with right internal jugular vein displacement due to large conglomeration, and no mediastinal lymphadenopathy.
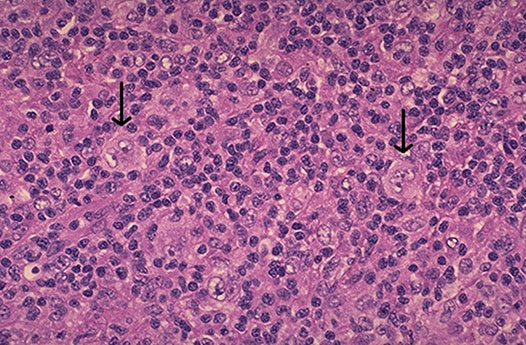
A biopsy of the right cervical lymph node and a bone marrow biopsy was obtained. Stains showed CD15 weakly positive, CD30 positive in lacunar cells, Pax-5 weakly positive, and CD20 negative to weakly positive.
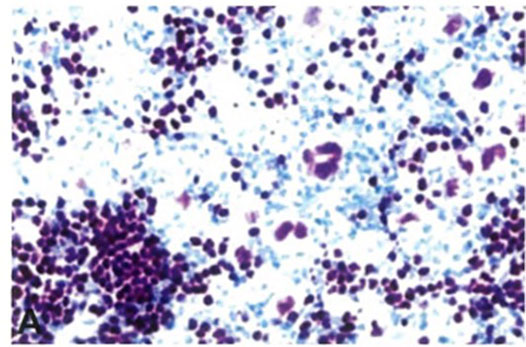
The following cell type was found on the lymph node and bone marrow biopsy2:
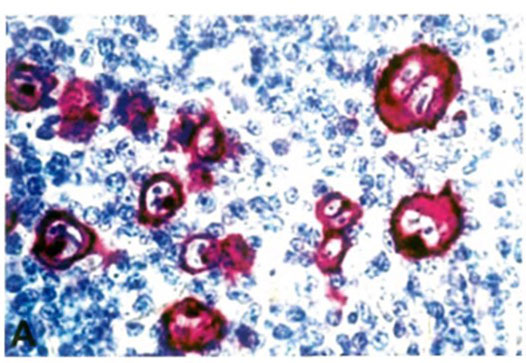
CD30: Membrane and cytoplasm staining
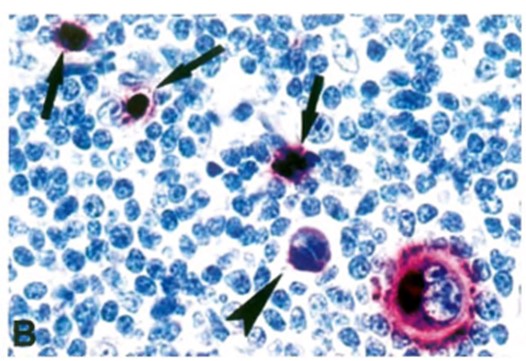
CD15: Membrane and perinuclear staining
PAX5: Stains the nuclei of these cells weakly

 Meet our Residency Program Director
Meet our Residency Program Director
