October 2023 – Presented by Dr. Erdembileg “Beke” Chuluunerdene (Mentored by Dr. Clayton LaValley)
Case Report: Diagnostic Challenges and Revelations in the Context of an Elevated Lipemic Index
Introduction and Clinical Presentation
A 69-year-old male patient, presented an intriguing case of asymptomatic hypoglycemia accompanied by an abnormally high lipemic index, reported as over 500+ mg/dL by two separate laboratory analyzers. Remarkably, visual inspection of the blood samples did not reveal the expected fat layer typically associated with such high lipemic indices, prompting a detailed investigation into the root cause of these abnormal results.
Medical History
A 69-year-old patient presented a multifaceted medical history alongside unusual laboratory findings. On April 11, 2023, his medical records indicated elevated serum protein levels and an increased Erythrocyte Sedimentation Rate (ESR). Additionally, he was diagnosed with Parkinson’s Disease, which was under active management. A notable aspect of his medical history included a thyroid mass. His past exposure to radioactive isotopes during the Chernobyl disaster raised concerns about potential long-term health implications. Furthermore, the patient was dealing with chronic renal failure, categorized as stage 3a. Importantly, there were no prior indications or diagnoses of any form of monoclonal gammopathy in his medical history.
Investigative Approach and Laboratory Findings
Given the unusual laboratory findings, a comprehensive approach was undertaken. This included revisiting the patient's medical history and conducting a series of specific laboratory tests aimed at identifying potential causes of the lipemic index anomaly.
A Protein Electrophoresis (PEP) was carried on left over plasma and revealed abnormal protein distribution (Figure 1), particularly in the gamma region of the electrophoresis pattern, suggesting the presence of a monoclonal protein. Additionally, the presence of beta bridging raised suspicions of altered coagulation factor levels, a possibility when plasma is utilized in PEP.
In light of these findings, we asked the patient to return to the hospital for repeat testing. Serum Protein Electrophoresis (SPEP) and Immunofixation Electrophoresis (IFE) were conducted, which identified an SPEP monoclonal protein concentration of 1.4g/dL and an IgM Kappa monoclonal protein. These results were instrumental in establishing a diagnosis of monoclonal gammopathy, a condition previously undetected in this patient.
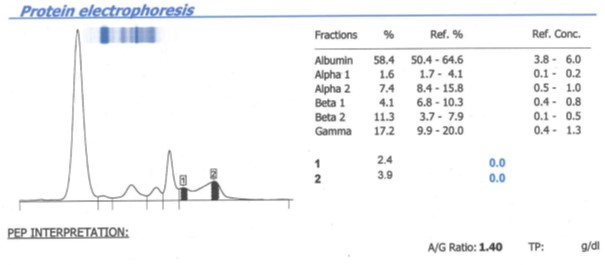
Figure 1. Analysis of Plasma Sample via Protein Electrophoresis (PEP). The graphic reveals two distinct regions of interest within the evaluated sample. Region 1 showcases the occurrence of beta-bridging, a common phenomenon when running plasma samples through PEP. In contrast, Region 2 suggests a potential gammopathy.
The correct answer is:
Explanation:
The patient's presentation aligns with Waldenström Macroglobulinemia (WM), a condition characterized by lymphoplasmacytic lymphoma (LPL) in the bone marrow and IgM monoclonal gammopathy in the blood. WM can present with symptoms related to hematopoietic tissue infiltration and the effects of monoclonal IgM, including hyperviscosity, which can lead to blurred vision, and the presence of lymphadenopathy, as seen in this patient. The diagnosis of WM is further supported by the presence of more than 10% LPL infiltration in the bone marrow biopsy, a key diagnostic criterion. Smoldering WM is a related but less advanced condition and typically lacks the symptomatic presentation seen in this case. IgM MGUS, Multiple Myeloma, and Chronic Lymphocytic Leukemia do not match the specific combination of symptoms, serum findings, and bone marrow biopsy results as described in the question.
Citation: Laubach JP, Rajkumar SV, Connor RF. "Diagnosis of Monoclonal Gammopathy of Undetermined Significance". In: UpToDate. Waltham, MA: UpToDate; 2022. Last updated September 8, 2022. Literature review current through October 2023.

 Meet our Residency Program Director
Meet our Residency Program Director
