‘Let’s get her to the OR now.’ Infant’s RSV exposes life-threatening heart defect
Pediatric nurse expresses gratitude after his co-workers save his daughter’s life
When Mathew Hipwell’s 3-year-old son, Everett, caught RSV (respiratory syncytial virus) — a common respiratory virus that can be dangerous for some infants and young children — in October of 2021, Hipwell urged him to steer clear of baby sister, Ellie. As a pediatric nurse at UC Davis Children’s Surgery Center, Hipwell knew his daughter was especially susceptible. Soon she was coughing, too.

Since it happened to be time for Ellie’s 2-month-old checkup, her mom, Bethany, took her to the UC Davis Health pediatrics clinic in Roseville. The staff determined Ellie had RSV, was too sick to get her immunizations and gave her a breathing treatment instead. Soon, she was on her way to UC Davis Children’s Hospital.
“The next thing I knew, my wife was calling me from the back of an ambulance,” Mathew Hipwell said. “I figured they would treat her for a few days, and we’d be good.”
That wasn’t the case.
RSV exposes life-threatening condition

When Ellie arrived at the UC Davis Pediatric Emergency Department, doctors heard a heart murmur. A chest X-ray later revealed she had an enlarged heart. Hipwell knew something else was going on. Ellie was immediately admitted to UC Davis Children’s Hospital.
When the team performed an echocardiogram the next morning, the Hipwells got an unexpected and frightening diagnosis: ALCAPA.
“The room started filling with people and I was wondering what was going on,” Bethany Hipwell said. “I was looking at Mathew to gauge his reaction. He was trying not to freak me out.”
“Cardiologist Jay Yeh, whom I know, came running in and said Ellie had ALCAPA,” Mathew said. “I have scrubbed into the pediatric OR [operating room] for 12 years. I knew exactly what ALCAPA was and just how serious it is.”
The room started filling with people and I was wondering what was going on.”—Bethany Hipwell, Ellie’s mom
ALCAPA stands for anomalous left coronary artery from the pulmonary artery. It’s a congenital heart condition that leaves the left side of the heart with deoxygenated blood.
In a normal heart, both coronary arteries branch from the aorta. With ALCAPA, while the heart is forming in the womb, the left coronary artery branches from the pulmonary artery instead of the aorta. The condition is hard to detect and if left untreated, has a mortality rate up to 90% within the first year of life.
“I can handle it … I can handle it”

An Army reservist and a medical professional for 30 years, Hipwell has seen a lot. His right arm is adorned with colorful tattoos representing his wife and each of his five children — four of whom are adopted — who he calls his “right arm”.
There are tattooed owls for Hipwell’s oldest daughters, a monkey for his son, a tribute to his wife, Bethany, plus a family crest for happiness. A whole sleeve, in fact.
Ellie’s tattoo was yet to be decided. Besides, there was no room in the sleeve for this surprise baby. He’d have to make room, but first things first.
“I was deployed most of my wife’s pregnancy and was home just three weeks before she delivered Ellie,” Mathew recalled. “We were so thrilled to have this baby. She’s our only biological child and the only newborn we have had. It was hard to wrap my brain around what was happening.”
It’s very hard to take off the nursing hat and put on the husband and parent hat, but I knew I had to.”—Mathew Hipwell, Ellie’s dad
Hipwell calls himself a “tough guy” but admits Ellie’s illness was one of the hardest things he’s had to face. Although he had the utmost confidence in the team he works with, he discovered what it’s like to deal with his own child’s health crisis.
“It’s very hard to take off the nursing hat and put on the husband and parent hat, but I knew I had to,” Mathew said. “I said to myself, ‘I can handle it, I can handle it.’”
More unexpected news
It was a whirlwind for the Hipwells.
“I thought I’d have time to process,” Mathew said. “Then everything was compressed into a tight timeline.”

Ellie was quickly transferred to the Pediatric and Cardiac Intensive Care Unit (PCICU). The first stop was the cardiac catheterization (cath) lab for a procedure to determine how well Ellie’s heart was working. The appointment was originally scheduled for the next day, with surgery two days later. Plans changed.
The cath lab procedure took place that afternoon. During the procedure, a video of her blood flow revealed another issue: a duplex kidney.
A duplex kidney is a problem with the urinary tract where there are two ureters — the long, narrow tubes that drain urine from your kidneys to your bladder — draining urine from a single kidney. Although it’s not life threatening and often doesn’t require treatment, this birth defect was just one more unexpected diagnosis.
Soon after the cath procedure, pediatric cardiothoracic heart surgeon Gary Raff walked into the room and said, ‘We’re not waiting. Let’s get her to the OR now.’”
Ellie’s heart function was poor after the catheterization study. I was concerned about keeping her stable. I did not see any advantage to waiting, only potential disadvantage.”—Gary Raff, pediatric cardiothoracic surgeon
“Ellie’s heart function was poor after the catheterization study. I was concerned about keeping her stable,” said Gary Raff, a pediatric cardiothoracic surgeon. “I did not see any advantage to waiting, only potential disadvantage.”
The UC Davis Pediatric Heart Center’s integrated team of surgeons, cardiologists, and nurses offers families the most sophisticated, specialized expertise. Hipwell knows this firsthand. But when he saw some of his staff members pushing the ECMO — a machine used in open-heart surgery to pump and oxygenate a patient's blood outside the body — reality hit.
“We take the most precious thing in people’s lives — their children — and perform surgery,” Hipwell said. “Even though I had an idea of what the team would be doing and was confident in their skills, I was still out of my mind stressed as Ellie’s dad.”
In good hands
Although he was overwhelmed, Hipwell knew it had to be especially stressful on the team having the life of a colleague’s child in their hands.

“Imagine a friend from work’s child you have to operate on,” Mathew said. “All I could say was I’m glad it’s you. It was pretty brutal for the team, but I knew they were going to do great … because I see it every day.”
Anesthesia technician, Cindy Lomperski, said this about the prospect of Ellie being the child in surgery.
“The minute kiddos come into the Children’s Surgery Center, we think of them like they are our own,” Lomperski said. “Ellie is like family. They all are.”
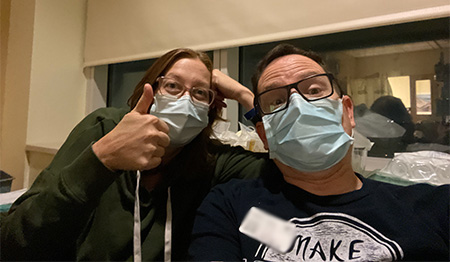
When Ellie was wheeled past the elevators in the Children’s Surgery Center — the place Hipwell spends every day helping other people’s children — he and Bethany gave her a kiss.
“Seeing my baby intubated with all the lines,” Mathew recalled, “that was probably the hardest for us. Everything was spinning, but I tried to keep it together.”
“Both of us ended up breaking down. We just stood there hugging each other and crying,” Bethany remembered.
Throughout the six-hour surgery, the team gave the Hipwells updates. The conversation was like those he has had with other families. It was hard to be on the other side, but Hipwell was reassured knowing exactly who was taking care of his daughter. To pass the time, he ordered Ellie some stuffed alpacas, a play on her ALCAPA diagnosis.
Expert care … and caring
When Raff completed the surgery – called translocation – he was thrilled with the result. He had successfully disconnected the anomalous left coronary artery from the pulmonary artery, repaired the damage and connected the artery to the aorta to restore normal blood flow. It was just before midnight when Ellie was back in the PCICU.
“My concern for Ellie was how quickly her left ventricular function would recover, as well as how much her respiratory viral infection would impact her,” Raff said. “Her recovery was as smooth as ALCAPA patients can have.”
Despite that, the Hipwells didn’t get much sleep during Ellie’s stay. An unexpected blessing perhaps, as they were able to experience another expert team in action.
“It was so nice listening to the team. It was like a NASCAR pit crew,” Mathew said. “They worked together seamlessly.”
Ellie’s parents were with Ellie every day and night as her condition improved over the next 10 days.
“The night shift nurse would check on Ellie and I could hear her singing, ‘You are my Sunshine,’” said Mathew. “It was ridiculously comforting to us.”
Singing seemed to comfort Ellie as well. When she was still intubated, a photo was taken as her parents sang her a song. Ellie smiled as she listened.

The smiles continue
When Ellie was able to go home, Hipwell said it was like getting a new baby back.
“I joked that it’s amazing what a working left ventricle will do for you,” Mathew quipped. “She was moving and grooving, playing with her brother, who, by the way, got an extra dessert for helping save his sister’s life by giving her RSV.”
“It’s scary to think about what could have happened had she not gotten sick,” Bethany added. “It’s amazing Ellie’s still here.”
Hipwell is reminded daily of the work of the incredible UC Davis Children’s Hospital team. All he has to do is look at Ellie — or the pink alpaca tattoo on his chest he got as a tribute to his youngest daughter. Plus, when he’s at work and sees the “Ellie Badge” worn by staff – made by a nurse colleague as a nod to the character Ellie in the movie “Up” – he can’t help but smile.

Ellie has been thriving since her surgery, requiring only cardiac checkups and to date, no treatment for her duplex kidney.
I firmly believe we provide world-class care to every child. For me, it was a really hard situation to go through as a dad, but I have my daughter to show for it and was able to bring even more passion to the job I love.”—Mathew Hipwell, Ellie’s dad
“I’ve known Ellie’s father Matt since he came to UC Davis. He and I spoke often of his other family members who are and were in the service,” Raff said. “Those Hipwells are tough and Ellie is a Hipwell.”
Mathew Hipwell agrees both about his mini me and the tremendous work of the UC Children’s Hospital staff — himself included.

“I firmly believe we provide world-class care to every child,” Hipwell said. “For me, it was a really hard situation to go through as a dad, but I have my daughter to show for it and was able to bring even more passion to the job I love. What we do is life altering, changing people’s lives for the better and helping children. I am where I’m meant to be.”
UC Davis Children's Hospital is the Sacramento region's only nationally ranked, comprehensive hospital providing care for infants, children, adolescents and young adults with primary, subspecialty and critical care. It includes the Central Valley's only pediatric emergency department and level I pediatric trauma center, which offers the highest level of care for its critically ill patients, as well as a level I children’s surgery center. The 129-bed children's hospital includes the state-of-the-art 49-bed neonatal and 24-bed pediatric intensive care and pediatric cardiac intensive care units. For more information, visit children.ucdavis.edu.