Real-time MRI captures wrists in motion
Moving images could revolutionize orthopaedic care and research
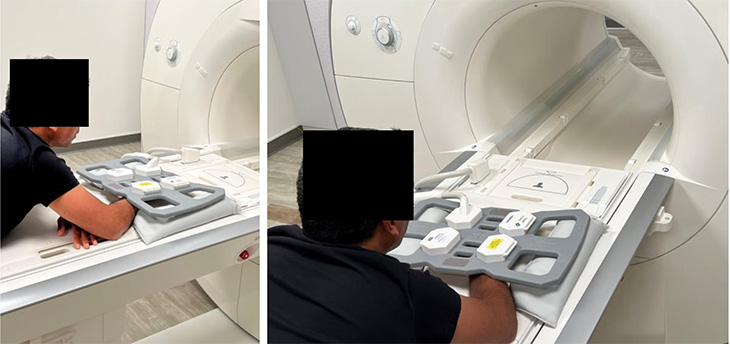
In a proof-of-concept study published in the British Journal of Radiology, UC Davis clinicians and researchers have shown that a new, low-field 0.55T MRI (magnetic resonance imaging) system can create clear videos of moving wrists. This emerging technology could provide important insights to improve diagnoses and better understand wrist anatomy.
“Moving images give us a new tool to diagnose wrist dysfunction, either during motion or when there is load on the joint,” said Abhijit Chaudhari, professor in the Department of Radiology and interim director of the UC Davis Imaging Research Center. “The wrist is highly complex, so the ability to visualize motion will have enormous impact.”
For decades, MRIs have provided excellent static images to inform diagnoses. However, the wrist has eight carpal bones and many ligaments, which can make it difficult for orthopaedists to assess motional dysfunction (also called dynamic instability) using still images alone. In some cases, patients have chronic wrist pain, but their doctors simply cannot determine the cause.
Moving images give us a new tool to diagnose wrist dysfunction, either during motion or when there is load on the joint. The wrist is highly complex, so the ability to visualize motion will have enormous impact.”—Abhijit Chaudhari, professor in the Department of Radiology
Wanting to solve this problem, Chaudhari, Robert Szabo, distinguished professor of orthopaedics and chief emeritus of hand and upper extremity surgery, and Robert Boutin, musculoskeletal radiologist and professor of radiology at Stanford University, have been working on real-time MRI for more than a decade. Their original efforts, in 2013, produced a meager two to three frames per second. Though ideal for still images, powerful three Tesla (3T) MRI machines produce visual artifacts, such as bands without signal, that can obscure wrist anatomy.
“We were doing all our work on 3T systems, and we realized we could not do much better because these system have limitations,” said Chaudhari. “Whenever movement is conducted within a high-field strength magnet, you disturb the magnetic field a lot, and that created artifacts in images that disrupt our ability to assess the joints.”
Developing a Better System
Chaudhari, Szabo and Boutin collaborated with Krishna Nayak, who directs the Dynamic Imaging Science Center at the University of Southern California and is a co-author on the new paper. Nayak and colleagues received a National Science Foundation grant to develop a 0.55T MRI system specifically for dynamic imaging.
In the current study, the team showed the 0.55T machine could produce diagnostic-quality images, either as stills or short, 78 frame-per-second movies. In addition, real-time MRI was incredibly fast. The research team produced high-quality videos in 5 seconds or less. This rapid capture means real-time MRI could improve care without adding significant cost.
“This approach allows us to study the trajectory of structures in an actively moving wrist,” said Szabo. “The dynamic pictures, along with standard, still MRI scans, show us specific wrist anatomy that had never been evaluated to this degree before. This has tremendous relevance to evaluate injuries and conduct further research into how the wrist functions.”
Imagine the difference between taking a movie of someone’s wrist while they are throwing a baseball compared to taking a still picture. Now imagine taking a moving MRI showing the inside of the wrist compared to an X-ray or static MRI. The added information will really improve care.” —Robert Szabo, distinguished professor of orthopaedics
A Wealth of Applications
In addition to advancing real-time MRI, the new 0.55T system could provide much-needed clinical versatility. The magnetic field does not extend far beyond the machine, eliminating the risk of disturbing metallic devices in the room. The instrument could also help patients with surgical implants, who currently cannot use high-field MRIs. Also, the machine has a smaller footprint, allowing it to be placed in smaller rooms.
“This could be quite beneficial for intraoperative applications, in which you take the patient out of the scanner and immediately perform the intervention,” said Chaudhari. “The applications of these low-field scanners continue to expand.”

In addition, there are still unanswered questions about how the wrist functions. Real-time MRI is now being used by the team to investigate wrist mechanics. Still, orthopaedists are most excited by the ability to clinically observe wrists in motion.
“Using this technique before and after wrist reconstructive surgery would allow us to see if our techniques restore normal anatomy in our patients,” said Szabo. “Imagine the difference between taking a movie of someone’s wrist while they are throwing a baseball compared to taking a still picture. Now imagine taking a moving MRI showing the inside of the wrist compared to an X-ray or static MRI. The added information will really improve care.”
Additional co-authors on the paper include Christopher Bayne of UC Davis, Yongwan Lim of the University of Southern California, Sophia X. Cui of Siemens Medical Solutions, and Robert Boutin of Stanford.
This study was supported by the National Science Foundation Grant MRI-1828736 and Siemens Healthineers.