Asthma in Children and Teens
Asthma medications
Medications have a variety of names; please verify with your pharmacist or health care provider which is quick relief and which is long acting.
Quick Relief Medications (Rescue):
These medications give your child quick relief of his or her symptoms. Your child should take these medications at the first sign of any asthma symptoms. Rescue medications do not replace the need for daily use of long term control medications.
Albuterol (ProVentil, Ventolin or ProAir) or Xopenex (levalbuterol):
- A reliever medication opens airways in the lungs. It relaxes the muscles in and around the airways that tighten during asthma attacks.
- Albuterol can be given by using an inhaler or a nebulizer.
- Inhaled albuterol works within five minutes and has very few side effects.
- Albuterol relieves symptoms, but cannot reduce or prevent the swelling that causes the symptoms.
- Normal side effects for this type of medication include jitteriness, trembling or increased heart rate.
Long Term Control Medications (Maintenance):
These medications are taken every day to prevent symptoms and asthma attacks. These medications reduce swelling and inflammation inside your child’s airway. This makes the airways less sensitive and less likely to react to triggers. These medications will not relieve symptoms during a breathing emergency!
Inhaled Corticosteroids:
- A controller medication used for patients with persistent asthma.
- These medications are most effective when taken every day, even when your child does not have symptoms.
- This medication is non-habit forming and goes directly to your child’s lungs where it is needed most.
- Be sure to rinse your child’s mouth out with water after using these medications, to prevent infections in the mouth.
Other Controller Medications:
- Your child may need other medications to help prevent swelling of the airways, such as Singulair (montelukast).
Oral Corticosteroids (liquid or tablet):
These medications are used for asthma attacks to reduce swelling of the airways and prevent the episodes from getting even more severe. This medication is given for a short time, usually five days.
-
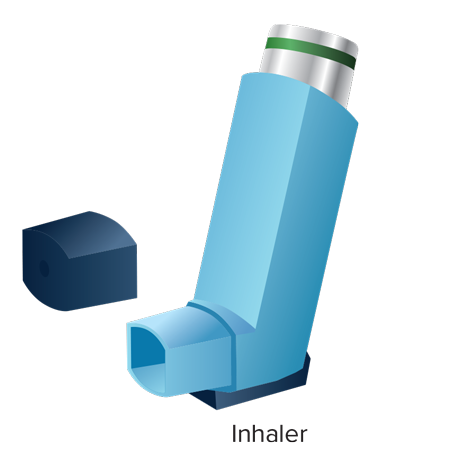
Inhaler
- A metered dose inhaler is a hand held device that delivers medication right to your child’s lungs where it is needed.
- Both quick relief and long-term control medications can be delivered with an inhaler.
- Remember to shake your child’s inhaler for 5 to 10 seconds before each use and have your child hold their breath for 10 seconds after the release of the medication to allow the medication to reach deeply into their lungs.
-
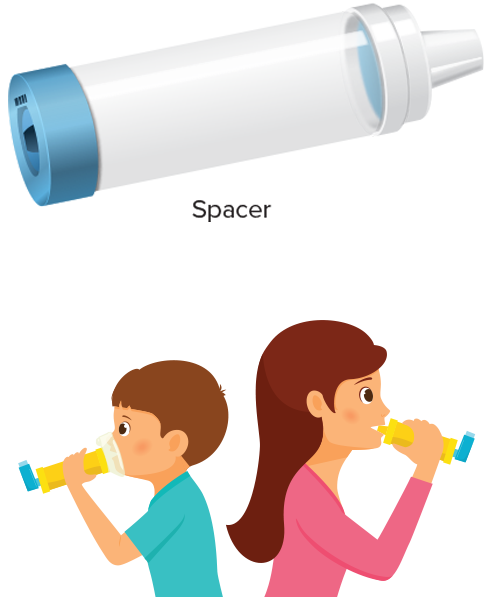
Spacers
- A spacer is a device that is attached to an inhaler.
- This device holds the medication in its chamber to help your child get more of the medication.
- Your nurse or respiratory therapist will teach you how to properly use the spacer device.
- Younger children or children who have trouble holding their breath may need a spacer with a mask.
- If your child is unable to hold their breath, you should hold the mask with spacer over their mouth and nose until they have taken at least 5-10 breaths.
- Some inhalers are “breath-actuated” and do not require use of a spacer. The medicine is delivered when your child takes a breath from the inhaler.
- Breath-actuated inhalers are only appropriate for some older children, so your doctor or medical provider will need to chose the right inhaler carefully.
-

Nebulizers
- A nebulizer provides medication to your child through a small, steady mist.
- Your child simply breathes in and out normally through a mask or mouthpiece connected to the nebulizer.
- This is sometimes used with infants and young children.
- If your child requires a nebulizer at home, you will be taught how to use and care for the equipment.
-

Peak Flow Meter
- The peak flow meter is a simple tool that can be used daily as an early warning tool for your child’s asthma. Any child over the age of five can use a peak flow meter.
- The peak flow meter measures how well your child’s airways are working.
- Your nurse or respiratory therapist will show you how to use a peak flow meter. You will be able to take one home to help monitor your child’s asthma.

