Fetal Care and Treatment Center
Twin-to-twin transfusion syndrome
What is twin-to-twin transfusion syndrome?
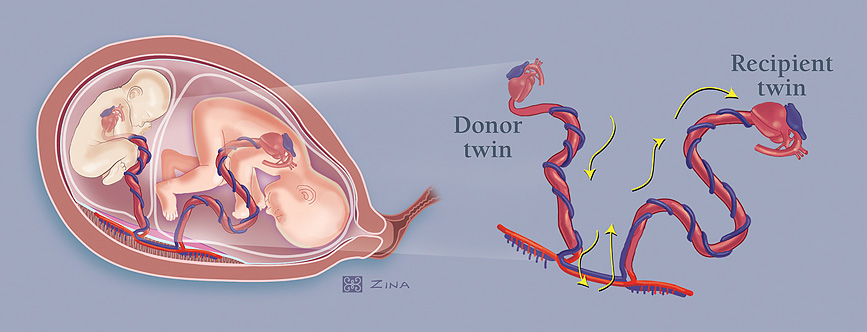
Twin-to-twin transfusion syndrome affects pregnancies with twin fetuses sharing one placenta, called monochorionic pregnancies. Blood passes disproportionately from one baby to the other through connecting blood vessels within their shared placenta.
One fetus — the recipient twin — gets too much blood, overloading its cardiovascular system and putting it at risk of heart failure. The recipient twin responds to the overload of blood by producing excess amniotic fluid.
The other baby, the donor twin, doesn’t get enough blood, leading to low amniotic fluid and poor fetal growth, putting it at risk of severe anemia.
Diagnosis
The key diagnostic tool for both shared placenta and twin-to-twin transfusion syndrome is ultrasound.
First, the presence of a shared placenta is confirmed using ultrasound findings. Twin-to-twin transfusion syndrome is then diagnosed by observation of an unequal amount amniotic fluid on either side of the dividing fetal membrane.
Once diagnosed, the condition’s severity is rated using what is known as the Quintero Staging System:
- Stage I: the donor twin’s bladder is visible by ultrasound
- Stage II: that bladder is collapsed and no longer visible by ultrasound
- Stage III: fetal Doppler studies, a type of ultrasound used to assess blood flow in the umbilical vein and arteries, are critically abnormal, often showing a reverse flow of blood between heartbeats as the donor sends blood to the recipient
- Stage IV: fetal heart failure is present
- Stage V: demise of either twin
Treatment
The pregnancy is monitored with serial ultrasound examinations. If twin-to-twin transfusion syndrome is diagnosed in its earliest stages, some physicians will recommend a wait-and-see approach.
Amnioreduction may be necessary to remove excess amniotic fluid from the recipient’s sac via a needle placed using ultrasound guidance. Because this approach does not treat the underlying cause, amniotic fluid excess may recur, resulting in the need for multiple amnioreductions.
Laser ablation utilizes an operative fetoscope to divide and seal off the interconnected blood vessels on the surface of the common placenta. Because vascular connections between the two fetuses are sealed, no further blood exchange between the fetuses takes place.
Outcomes
With early detection and laser ablation, there is a 65 percent chance of having two surviving babies and an 85 percent chance that one of the twins will survive. All babies should be completely evaluated after birth by neonatal specialists for concerns related to their hearts, kidneys and brains.
Contact us or make a referral
Physicians, patients and families can contact the Fetal Care and Treatment Center to find out more about our fetal care services.
Wondering about what types of conditions should be referred to us? View list of conditions to refer.
Referring physicians from other facilities, please use our Fetal Care and Treatment Center Referral form to refer patients and request services.
UC Davis Children’s Hospital
4301 X Street, 1st Floor, Suite 1501
Sacramento, CA 95817
The Fetal Care and Treatment Center is located within UC Davis Children’s Hospital.
View map and directionsarrow_forward

