September 2021 – Presented by Dr. Ryan Thomas (Mentored by Dr. Kurt Schaberg)
Case Presentation
A 50-year-old male with a known medical history significant for obesity, alcohol use, and hypertension was transferred from a community medical center for ICU-level management of sepsis with hemodynamic instability. After being stabilized, the patient complained of abdominal pain with melena. Imaging showed severe wall thickening of the ascending colon with adjacent inflammatory changes and possible pneumatosis. These findings were concerning for ischemic colitis versus an infectious or inflammatory colitis, and the patient was taken to the OR by acute care surgery. Intra-operatively, he was noted to have cecal perforation with ascending colon necrosis. An ileocecectomy was performed. Gross examination of the resection specimen revealed pale gray-tan to focally hemorrhagic necrosis involving the distal small intestine, the ileocecal valve and cecum, and midway through the segment of proximal colon, as well as the attached peri-colonic adipose tissue and small intestinal mesentery (Figure 1). Histologic sections revealed necrotic intestinal tissue with the findings shown in Figure 2, Figure 3, and Figure 4.

Figure 1: Gross examination of the ileocecectomy specimen showed necrotic and hemorrhagic areas (white arrows) involving the walls and surrounding tissues of the ascending colon and ileum.
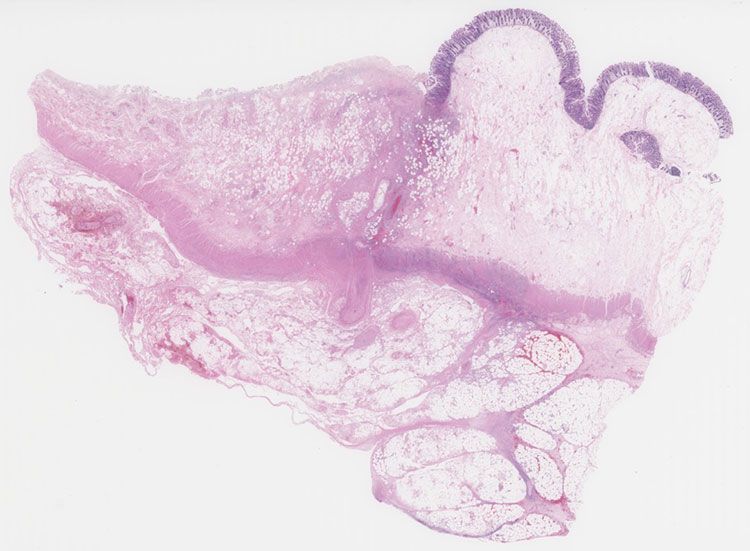
Figure 2: Representative section of ascending colon (whole slide fit to view)
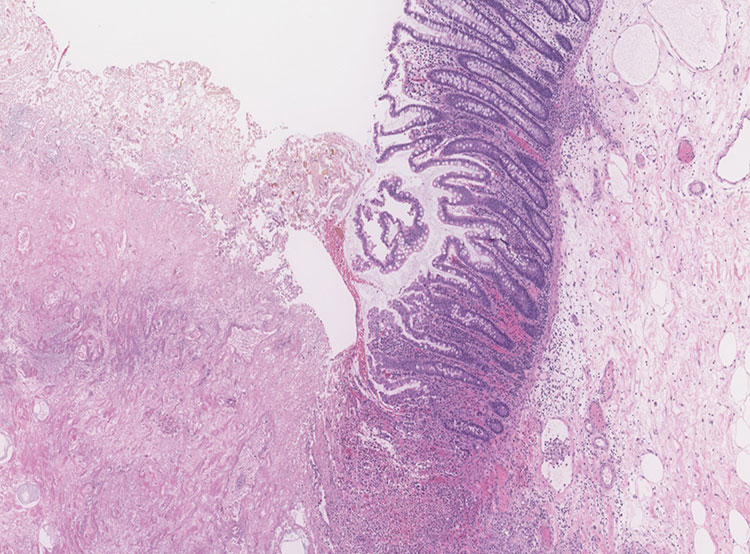
Figure 3: Representative section of ascending colon (40x magnification)
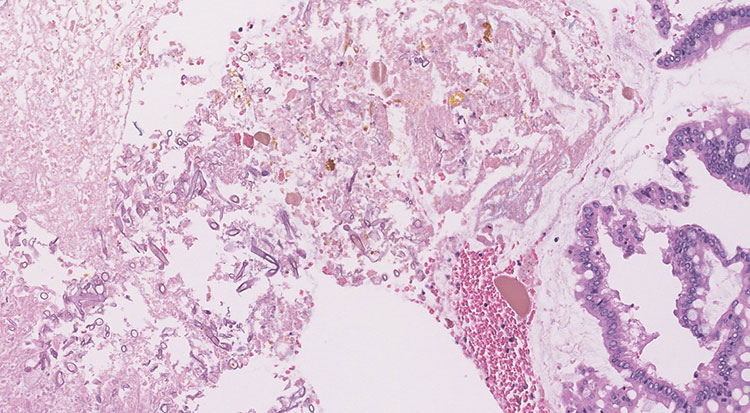
Figure 4: Representative section of ascending colon (200x magnification)

 Meet our Residency Program Director
Meet our Residency Program Director
