UC Davis lab develops fetal oximetry device to prevent unnecessary C-sections
Fetal hypoxia, a condition that occurs when the fetus is deprived of an adequate supply of oxygen, is one reason obstetricians may perform a Caesarean section (C-section). Currently, obstetricians use electronic fetal heart rate monitoring (EFM) during labor and delivery to assess fetal well-being. As of 2016, data published in Clinical Obstetrics & Gynaecology showed that 30% of babies delivered in hospitals in the U.S. are detected as potentially hypoxic, but 60% of those detections are false alarms that can lead to unnecessary C-sections.
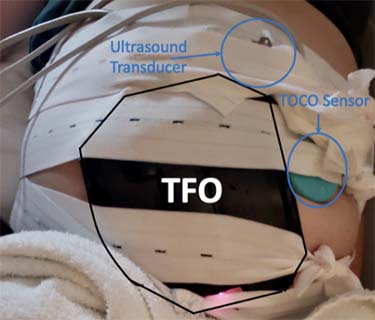
UC Davis electrical and computer engineering professor Soheil Ghiasi's lab has built a specialized device to measure a baby’s blood oxygen saturation levels non-invasively. It’s called a transabdominal fetal pulse oximeter (TFO.) A new father himself, Ghiasi says the birth of his young daughter inspired this research. The works supported by grants from the National Science Foundation and the National Institutes of Health.
Ghiasi expects this technology wil be adopted by many medical facilities worldwide.
"From my observations, nurses and obstetricians are well-trained on how to use fetal monitoring devices, and this is something to which they can easily adapt,” Ghiasi said. “Placing TFO on the abdomen is similar to placing ultrasound transducers currently used for fetal monitoring at hospitals. A friendly graphical user interface can provide easy access to fetal oxygen saturation numbers outputted by the TFO and help with the adaptation. Additionally, TFO is composed of off-the-shelf components and is relatively low-cost.”
Testing accuracy in pregnant ewes
The research team is currently testing the accuracy of the fetal oximeter in pregnant ewes, in collaboration with Diana L. Farmer, chair of the UC Davis Department of Surgery and an internationally renowned fetal and neonatal surgeon at UC Davis Health.
The collaboration also includes Herman Hedriana and Aijun Wang of UC Davis Health; Weijian Yang, Naoki Saito, Andre Knoesen and Vivek Srinivasan at UC Davis; and M. Austin Johnson, previously at UC Davis Health and now at the University of Utah.
"We have done 13 animal studies with various prototypes of the TFO device since 2019, thanks to all of these collaborators. Our latest animal study showed that our TFO can measure fetal oxygen saturation with about 10% mean absolute error," said Begum Kasap, a Ph.D. student working on the project.
Accessing reference oxygen saturation values is necessary to characterize and calibrate any pulse oximetry system. To accomplish this, researchers can draw blood from sheep fetuses during the study to compare actual fetal blood oxygenation data with observations from the TFO technology. The procedure follows a strict protocol, approved by the UC Davis Institutional Animal Care and Use Committee, where the sheep are under anesthesia.
Prenatal testing in humans
The new oximeter was tested on a small group of humans in 2021 in collaboration with Herman Hedriana, director of Maternal-Fetal Medicine at UC Davis Health. Healthy near-term pregnant patients coming in for their non-stress test (NST) visits were enrolled in the study, which was conducted at UC Davis Medical Center.
The evaluation of TFO for use in prenatal testing is an important step towards its integration into hospitals for fetal monitoring during labor and delivery. However, because researchers cannot draw blood as frequently from human fetuses, the performance of TFO in humans is evaluated using proxy metrics, such as fetal heart rate and maternal heart rate.
"We had a mean absolute error of 6.3 beats per minute (bpm) for fetal heart rate with our technology and a mean absolute error of 1.3 maternal heartbeats per minute across three patients. We want an error of below 5 bpm for a clinical application, so we are working on this," Kasap said.
The device has been tested on patients with darker skin tones, and it has proven less accurate than those with lighter skin.
"More light gets absorbed while passing through the body of someone with a darker skin tone, so less light is reflected to the surface, making it harder to obtain observations," Kasap said. To correct this, they've made it possible to adjust the brightness of the LED light source. However, there's a safety-related upper limit on brightness to avoid the possibility that the LED in contact with someone's body will overheat.
The researchers are developing another prototype that is less sensitive to 'noise' - other things the sensors pick up that have nothing to do with fetal blood oxygenation - which can work with lower levels of light. This year, Ghiasi, Kasap and their many collaborators will carry out further oximeter tests during labor and delivery in both animals and humans.
Related links
UC Davis startup develops monitor that measures baby’s blood oxygen saturation in the womb