What's at stake with federal research funding cuts
Federal funding enables UC Davis researchers to improve lives across fields — from medicine to food, agriculture to technology
From ALS to Alzheimer’s disease to cancer, diabetes and other serious conditions, UC Davis Health researchers are working on discoveries and therapies that offer hope. Much of this research is thanks to a longstanding partnership with the federal government.
That partnership has powered decades of groundbreaking research on fundamental science and clinical trials, helping patients to manage symptoms, improve quality of life and move closer to cures.
It’s not just medicine. Across the University of California, Davis, federally funded research has also led to innovations in agriculture, food safety, and environmental sustainability.
Researchers have learned how to make strawberries more drought-resistant and developed flood-resistant rice to create a more reliable food source for tens of millions of people. They also discovered that feeding seaweed to cattle can significantly cut methane emissions, to name just a few advances.
For decades, the federal government has relied on top-tier research universities like UC Davis to carry out laboratory research, clinical trials and fundamental science that advance human, animal and planetary health, make the food supply safer and healthier, and improve our understanding of the world.
Much of this research happens with little fanfare.
But since the new administration took office early this year, the federal government has retreated from the partnership that makes this research possible, endangering medical and scientific breakthroughs, economic growth and the United States’ leadership as the global scientific powerhouse. Dozens of federal grants already have been canceled, and the federal government has moved to cut administrative support for ongoing work.
“Critics of basic research call the work wasteful, suggesting it’s a luxury we can’t afford in a time of tight national budgets,” UC Davis Chancellor Gary S. May said in a recent “Chancell-ing” column. “However, this seemingly undirected exploration leads to unpredictable breakthroughs that create new industries and solve problems we didn't even know we had.”
At UC Davis, federal funding is the largest source of research support. According to a newly released report, the federal government accounted for about 47% of research funding to UC Davis in fiscal 2024-25, ahead of state and private industry funding.
Every dollar spent on research at UC Davis generates more than $2 for California's economy. The university’s total spending of $955 million on academic research generates $2.1 billion statewide, and 4,316 jobs in academic research lead to a total of 9,577 jobs statewide, according to an economic impact analysis released earlier this year.
In the last fiscal year, UC Davis had a surge in records of invention, or ROIs, filing 187, up from 140 the prior year. An ROI serves as the initial step in evaluating the potential for patents and commercialization.

From Labs to Lives: The real-world impact of research
In February, UC Davis launched a campaign to increase public understanding of the value of university-led research. From Labs to Lives spotlights the researchers who are working to improve lives through their work across fields — from medicine to food, agriculture to technology.
“Without continued funding, we risk losing critical insights into how stress shapes family health, leaving communities vulnerable to the long-term effects of chronic stress,” said Rebecca Calisi Rodríguez, an associate professor in the College of Biological Sciences who studies how chronic stress affects parents’ brain health.
“If we stop funding research, we won’t just lose knowledge. We’ll lose the next generation of scientists who would have made the world a better place.”
What follows are a few examples of groundbreaking research at UC Davis made possible by federal funding.
How diabetes research can improve children's brain health
A collaboration between UC Davis psychologist and pediatric endocrinologist looks at the connections between Type 1 diabetes and cognitive decline in children.
With a $2.5 million grant from the National Institute of Diabetes and Digestive and Kidney Diseases, Simona Ghetti, a professor of psychology in the College of Letters and Science, and Nicole Glaser, a pediatric endocrinologist at UC Davis Health, are building on their research on diabetic ketoacidosis in children.
“Well-controlled Type 1 diabetes does not necessarily result in cognitive difficulties,” said Ghetti, “but there are several complications of diabetes that might alter the brain metabolism to the point that it might really have long-term consequences.”
Ghetti and Glaser are leading the new study as part of a national research consortium funded by the National Institute of Diabetes and Digestive and Kidney Diseases. UC Davis is one of 13 sites that will follow about 1,000 children from several children’s hospitals in the U.S. for two years.
The research teams are diverse and will explore factors that range from variability in blood sugar levels and changes in markers of inflammation to whether children get enough sleep or have access to diabetes care. Each aspect of the project will take a different approach to understanding how Type 1 diabetes contributes to neurocognitive difficulties in children. This will be the first large-scale study to follow children with Type 1 diabetes over time to see how they progress in their neuro-cognitive development.
“There's a lot of different expertise and hopefully we will not miss anything that is important,” said Ghetti. “When you do a study this big, you don't want to miss anything because this is a one-time opportunity.”
Understanding diabetic ketoacidosis
Ghetti and Glaser are building on their years of collaborative research related to diabetic ketoacidosis. In 2020, they published the results of a randomized controlled trial that included nearly 800 children from 6 to 18 years old to compare cognition between diabetic children with and without diabetic ketoacidosis.
Children with who experienced a single episode of diabetic ketoacidosis had a slightly lower intelligence quotient. They also had more trouble with a task remembering the colors of items and with remembering and repeating numbers back in order.
“Once we better understand these factors, we can develop ways to address them to prevent cognitive decline,” said Glaser.

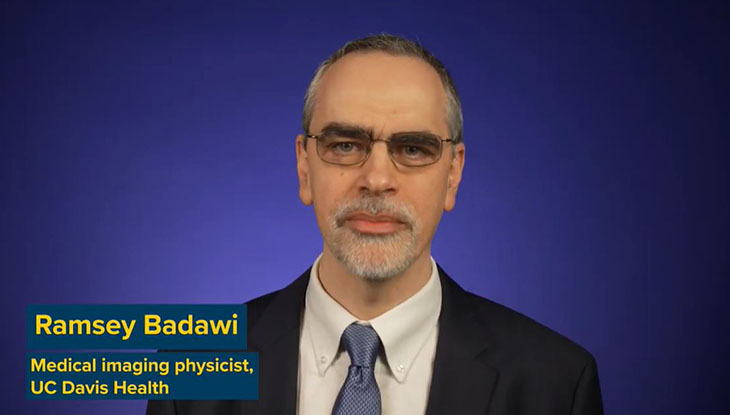
The world’s first total-body PET scanner, EXPLORER
A decade ago, Ramsey Badawi, professor of biomedical engineering and radiology, and Simon Cherry, distinguished professor emeritus of biomedical engineering and radiology, were awarded $15.5 million as a Transformative Research Award from the National Institutes of Health, or NIH, to build the world’s first total-body positron emission tomography, or PET, scanner.
“The vision of the project is to solve two fundamental limitations of PET as it is currently practiced,” Cherry said at the time. “The first is to allow us to see the entire body all at once. The second huge advantage is that we’re collecting almost all of the available signal, which means we can acquire the images much faster or at a much lower radiation dose. That’s going to have some profound implications for how we use PET scanning in medicine and medical science.”
The duo went on to build the scanner, now known as the EXPLORER total body PET scanner. They received approval from the Food and Drug Administration in 2018 for the scanner, which can capture a 3D picture of the whole body at once, allowing more accurate imaging while reducing radiation exposure. As the scan produces breathtaking image quality, the technology can be particularly helpful to researchers studying cancer that has spread beyond a single tumor site, inflammation, infection, immunological or metabolic disorders and many other diseases.

Using total-body PET scans to tackle long COVID
In August, researchers announced a $3.2 million grant over four years from the National Institute of Allergy and Infectious Diseases, part of the NIH, to use the EXPLORER total-body PET scanner to get a better understanding of long COVID disease in collaboration with UC San Francisco.
About 1 in 10 COVID-19 survivors develop a range of long COVID symptoms that can last from months to years. How and why these symptoms develop isn’t completely known, but they have been linked to activated immune T cells getting into organs and tissues. Researchers also have linked long COVID to damage to the inner lining of blood vessels. These events can be related, because blood vessels become leaky when T cells are activated nearby, but may also be coincidental because leaky blood vessels allow more immune cells to leave the blood and enter tissues.
Negar Omidvari, assistant project scientist at the UC Davis Department of Biomedical Engineering and principal investigator on the grant, will use total-body PET technology, originally developed by Cherry and Badawi at UC Davis, and kinetic modeling to look at both processes simultaneously in patients with long COVID.
“Total Body PET has created, essentially, a whole new industry,” Badawi said in an interview for From Labs to Lives. “But without the kick-starting of the federal health care dollars to really turn that idea into practice, I’m not sure it would ever have happened.”


Brain-computer interface allows man with ALS to ‘speak’ again
A groundbreaking brain-computer interface (BCI) developed by UC Davis Health researchers translates brain signals into speech with up to 97% accuracy — the most accurate system of its kind.
Neurosurgeon David Brandman implanted sensors in the brain of Casey Harrell, a participant with severe speech impairment due to ALS, also known as Lou Gehrig’s disease.
Harrell was able to communicate his intended speech within minutes of activating the BCI system. A paper about the work, part of the BrainGate clinical trial, was published in the New England Journal of Medicine.
The technology is being developed to restore communication for people who can’t speak due to paralysis or neurological conditions such as ALS. It can interpret brain signals when the user tries to speak and turns them into text that is ‘spoken’ aloud by the computer.
“This technology is transformative because it provides hope for people who want to speak but can’t,” said Brandman, in a press release last year.
Brandman is an assistant professor of neurology. He and neuroscientist Sergey Stavisky are co-principal investigators on the BrainGate2 study. They also co-direct the UC Davis Neuroprosthetics Lab.
Stavisky said the first test of the system with the participant was emotional for all involved.
“The first time we tried the system, he cried with joy as the words he was trying to say correctly appeared on-screen. We all did,” said Stavisky, an assistant professor in the Department of Neurological Surgery.

Moving into ‘real-time’ speech
Now, Stavisky and Brandman have developed the investigational brain-computer interface to hold real-time conversations. In a study published in Nature, they demonstrate how the new technology can instantaneously translate brain activity into voice as a person tries to speak — effectively creating a digital vocal tract with no detectable delay.
In the BrainGate 2 clinical trial, the BCI allowed Harrell to not only speak with his family in real time, but change his intonation and “sing” simple melodies.
“This new real-time voice synthesis is more like a voice call,” Stavisky explained in a press release this year. “With instantaneous voice synthesis, neuroprosthesis users will be able to be more included in a conversation,” he said.
The BCI study is funded largely by a $2.7 million grant from the U.S. Department of Defense and a $2.3 million grant from the NIH Office of the Director .
“Not being able to communicate is so frustrating and demoralizing. It is like you are trapped,” Harrell shared. “Something like this technology will help people back into life and society.”




