Study aims to better understand reasons behind common type of heart failure
Although more than 3 million people in the U.S. are diagnosed with HFpEF each year, the condition is difficult to detect, and treatment options are limited
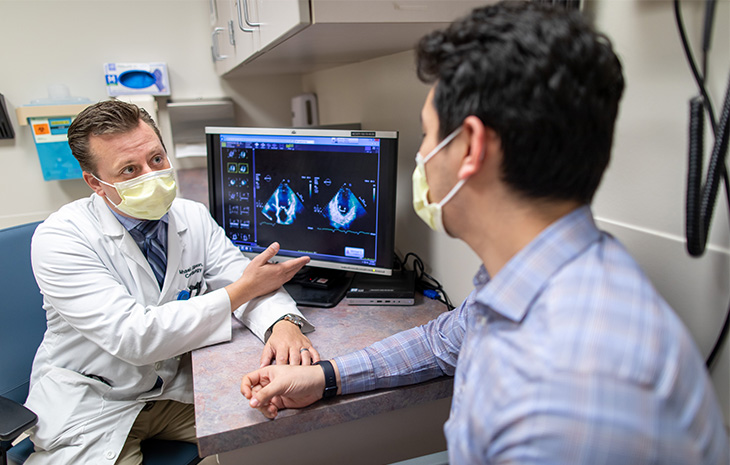
UC Davis Health cardiologists have received a $1.5 million grant to further explore a common type of heart failure and develop a more targeted treatment for it.
Heart failure with preserved ejection fraction (HFpEF) is a syndrome where the heart’s lower left chamber pumps out less blood than the body requires. Although the condition has several symptoms, such as shortness of breath, it is difficult to properly diagnose.
HFpEF also has few proven therapies and a lack of clear definitions for its subtypes, so the condition has contributed to misdiagnosis and poor outcomes in patients.
But soon, UC Davis Health cardiologists will be able to better evaluate HFpEF with a precision medicine approach, thanks to the grant from the National Institutes of Health (NIH) to classify this heart failure into different subtypes for more precise treatments.
The grant is part of the NIH's HeartShare program, a multi-institutional research effort that seeks to characterize the mechanisms driving HFpEF and identify new therapies.
“It is an incredible honor for us to be part of the HeartShare grant from the NIH, which allows us to continue our research to improve the classification of HFpEF and better understand the mechanistic underpinnings of this heterogeneous disease,” said Nipavan Chiamvimonvat, the Roger Tatarian Endowed Professor in Cardiovascular Medicine at UC Davis Health and a co-principle investigator of the grant. “These results could provide us earlier identification of targeted interventions and improve patient outcomes.”
What is heart failure with preserved ejection fraction?
Previously known as diastolic heart failure, HFpEF occurs when the lower left chamber of the heart is unable to relax and fill properly during the diastolic phase. The condition causes less blood than normal to be pumped throughout the body.
“HFpEF accounts for nearly half of all heart failure cases, adding up to at least three million diagnoses in the United States each year, and is associated with a five-year mortality of 30-60%,” explained Javier Lopez, the medical director of the Cardiac Rehabilitation Program and a co-principle investigator of the grant.
With HFpEF, the lack of normal relaxation of the heart muscle increases pressure inside the ventricle. This increased filling can cause fluid buildup in the lungs, leading to shortness of breath, fatigue, irregular heartbeat and, ultimately, heart failure.
“The incidence of HFpEF is rising in prevalence and will soon become the most common type of heart failure due to our aging population and the ongoing epidemics of obesity, diabetes, and hypertension,” explained Martin Cadeiras, medical director of the Heart Failure, Transplantation and Mechanical Circulatory Support Program at UC Davis Health and co-principle investigator of the grant. “Moreover, the current therapeutics for HFpEF have shown limited effectiveness, increasing the urgency to understand the mechanisms of this disease.”
HeartShare study

For the HeartShare Study, researchers are recruiting participants with and without heart failure. Participants will be monitored for a four-year period, starting with a survey upon enrollment to learn about their demographics, health, and family history, as well as a complete clinical evaluation to assess their heart function.
“Our hope is this research will offer new hope and excitement to transform care for patients with heart failure with preserved ejection,” said Imo Ebong, a UC Davis advanced heart failure and transplant cardiologist, and a co-investigator on the study.
Additional UC Davis co-investigators include Jason Adams, Kwame Atsina, Michael Gibson, Anne Knowlton, David Liem and Padmini Sirish of the Department of Internal Medicine; Nicholas Anderson of the Department of Public Health Sciences; Simon Cherry of the Department of Biomedical Engineering; Ramsey Badawi and Guobao Wang of the Department of Radiology; Bruce Hammock of the Department of Entomology; and Leighton Izu of the Department of Pharmacology.




