High blood pressure in your 30s associated with worse brain health in your 70s
New study suggests treating hypertension in young and middle-aged adults may help prevent dementia and Alzheimer’s
Key points:
- Study shows high blood pressure in early adulthood is associated with worse brain health in late life.
- Men, compared to women, may be more vulnerable to the detrimental effects of high blood pressure on the brain for some brain regions.
Having high blood pressure in your 30s is associated with worse brain health around age 75, especially for men, according to a new UC Davis study.
The research, published this week in JAMA Network Open, compared magnetic resonance imaging (MRI) brain scans of older adults who had high blood pressure between the ages of 30 to 40 with older adults who had normal blood pressure.
The researchers found that the high blood pressure group had significantly lower regional brain volumes and worse white matter integrity. Both factors are associated with dementia.
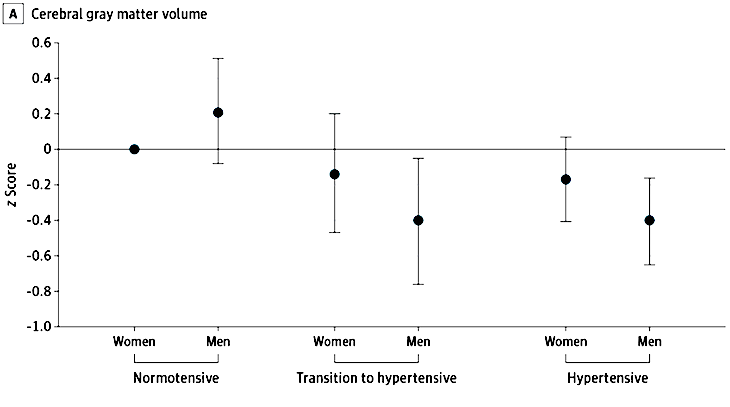
The research also showed that the negative brain changes in some regions — such as decreased grey matter volume and frontal cortex volume — were stronger in men. They note the differences may be related to the protective benefits of estrogen before menopause.
“Treatment for dementia is extremely limited, so identifying modifiable risk and protective factors over the life course is key to reducing disease burden,” said first author Kristen M. George, an assistant professor in the Department of Public Health Sciences.
“High blood pressure is an incredibly common and treatable risk factor associated with dementia. This study indicates hypertension status in early adulthood is important for brain health decades later,” George said.
High blood pressure prevalent in U.S.
High blood pressure, also known as hypertension, is blood pressure that is higher than normal. A normal blood pressure level is less than 130/80 mmHg. The Centers for Disease Control and Prevention estimates that 47% of adults in the United States have hypertension.
The rate of high blood pressure varies by sex and race. About 50% of men have high blood pressure compared to 44% of women. The rate of hypertension is about 56% in Black adults, 48% in white adults, 46% in Asian adults and 39% in Hispanic adults. African Americans ages 35-64 years are 50% more likely to have high blood pressure than whites.
Methods
The researchers looked at data from 427 participants from the Kaiser Healthy Aging and Diverse Life Experiences (KHANDLE) study and the Study of Healthy Aging in African Americans (STAR). This provided them with health data from 1964 to 1985 for a diverse cohort of older Asian, Black, Latino and white adults.
They obtained two blood pressure readings from when the participants were between the ages of 30 to 40. This allowed them to determine if they had been hypertensive, transitioning to hypertensive or had normal blood pressure in young adulthood.
MRI scans of the participants conducted between 2017 and 2022 allowed them to look for late-life neuroimaging biomarkers of neurodegeneration and white matter integrity.
Results
Compared to participants with normal blood pressure, the brain scans of those transitioning to high blood pressure or with high blood pressure showed lower cerebral gray matter volume, frontal cortex volume and fractional anisotropy (a measure of brain connectivity). The scores for men with high blood pressure were lower than those for women.
This study truly demonstrates the importance of early life risk factors and that to age well, you need to take care of yourself throughout life — heart health is brain health."—Rachel Whitmer, professor, departments of Public Health Sciences and Neurology
The study joins a growing body of evidence that cardiovascular risk factors in young adulthood are detrimental to late-life brain health.
The researchers note that due to the sample size, they could not examine racial and ethnic differences and recommended interpreting results regarding sex differences with caution. They also note that the MRI data was only available from one time-point late in life. This can only determine physical properties like volumetric differences, not specific evidence of neurodegeneration over time.
“This study truly demonstrates the importance of early life risk factors and that to age well, you need to take care of yourself throughout life — heart health is brain health,” said Rachel Whitmer, senior author of the study. Whitmer is a professor in the departments of Public Health Sciences and Neurology and chief of the Division of Epidemiology. She’s also the associate director of the UC Davis Alzheimer's Disease Center.
“We are excited to be able to continue following these participants and to uncover more about what one can do in early life to set yourself up for healthy brain aging in late life,” Whitmer said.
Additional authors of the study include Pauline Maillard, Evan Fletcher, Dan M. Mungas and Charles DeCarli, UC Davis; Paola Gilsanz, Kaiser Permanente Division of Research; Rachel L. Peterson, University of Montana, Missoula; Joseph Fong and Elizabeth Rose Mayeda from UCLA; L. Barnes from Rush Medical College; M. Maria Glymour from UCSF.
Resources


