“As a doctor and a policymaker, I often hear the question ‘what it is about black and brown people’ that makes us more vulnerable to the virus?” California’s inaugural surgeon general Nadine Burke Harris, M.D., M.P.H., F.A.A.P., wrote in an essay titled “George Floyd’s Death Is Killing Me,” published in June on the online platform Medium.
“That question infuriates me.”
“The science makes clear how powerfully our experiences and environments shape our biology,” she wrote. “It has been clear for decades. Our daily experiences activate cascades of biological pathways… Racist oppression ensures that black and brown children bear a disproportionate burden of dehumanizing and traumatic experiences. Science shows it is sickening them and killing them.”
Like many UC Davis School of Medicine alumni, Burke Harris (M.D.,’01) has dedicated her career to closing gaps in health disparities, especially in regard to the intersection of emotional stressors and physical health. During the pandemic and the aftermath of George Floyd’s death, she has played a vocal role in California and beyond highlighting how pandemic stress can be of harm to all of us — and, when intertwined with the effects of systemic prejudice, especially so for communities of color.
Since founding a nonprofit health center serving San Francisco’s impoverished Bayview neighborhood in 2007, the pediatrician has emerged as a national expert on the lifetime health impacts of toxic childhood stress and the phenomenon of Adverse Childhood Experiences, or ACEs. Research suggests that people of color, of lower incomes, and LGBTQ identity are more likely to experience ACEs, which range from parental divorce to household substance and domestic abuse.
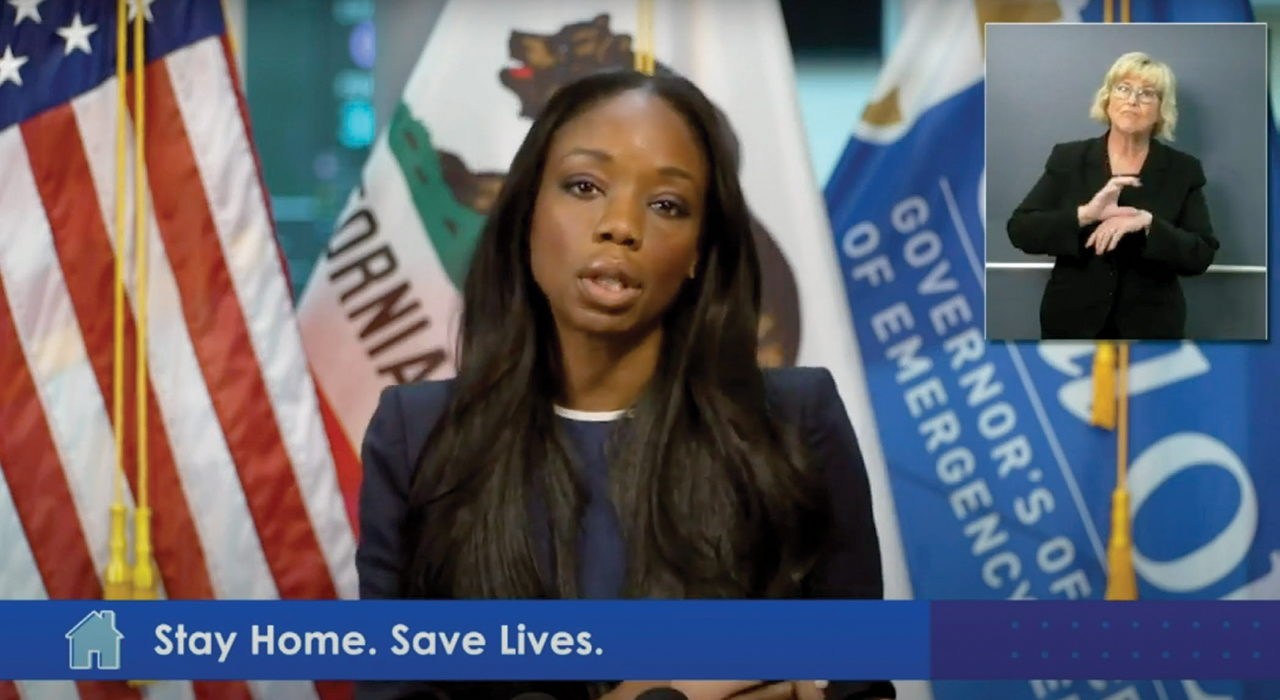
Expanding screening for ACEs, and advancing the science around them, has been a declared priority for Burke Harris since being appointed surgeon general by Gov. Gavin Newsom in January 2019. He also commissioned her to assist with the state’s response to pandemic-related mental health issues this spring; among other activities, her office created a sharable playbook of evidence-based resiliency tools to help with stress and emotional well-being, shared in outreach efforts and highlighted at an April pandemic news conference.
The role of racial disparities
In speaking about the importance of looking at racial disparities in health care, Newsom called Burke Harris to the podium while announcing, “This has been, quite literally, the cause of her life.” She stated that historically there has been medical mistreatment of African Americans, and emphasized the importance of identifying trusted messengers to communicate truthful messages.
At another point, she explained why the health effects of coronavirus go beyond infection: “It is important to recognize that stress related to the pandemic that many are feeling right now — compounded by the economic distress due to lost wages, employment and financial assets, plus school closures and sustained physical distancing — can trigger the biological stress response which also has an impact on our health and well-being,” she told Californians.
People who experience too much stress can be associated with changes in sleep patterns, appetite, mood, risk of substance abuse and family violence, she said. Physical symptoms can also include headaches, stomach pain, increased blood pressure and asthma.
People of color are already highly impacted by stress-related chronic conditions like hypertension, asthma and diabetes, Burke Harris has noted in media interviews, and she has expressed concern that new diagnoses or exacerbations caused by pandemic stress will likely impact those communities the most. They’d also be in line for a “double whammy” effect: besides causing physical harm in and by themselves, the conditions serve as additional risk factors or “core comorbidities” for COVID-19 complications as well.
As of late July, recent national data from the CDC showed that COVID-19 hospitalization rates for Indigenous and Black people were five times higher than for white people, and rates for Latinos are about four times higher than that of white people.
Full circle
And evidence shows that several kinds of chronic or comorbid conditions can be linked back to Adverse Childhood Experiences, Burke Harris has stressed both during the pandemic and throughout her career. Studies suggest the more ACEs a child has gone through, such as observing violence or being raised by a parent who abuses alcohol, the more likely that individual will suffer health risks later in life.
Children already exposed to ACEs are at increased risk of struggling during and after the pandemic, she told The New York Times in a May article “How to Keep Children’s Stress From Turning Into Trauma,” one of a number of related appearances in national media. And kids who were not at risk before COVID-19 may face new risks, because past safety nets and support networks may become overwhelmed or disappear.
California has passed legislation requiring that all Medicaid recipients be screened for ACEs, and in January began offering provider training and payments through the tobacco tax-funded ACES Aware initiative. Such screening will become even more important in the wake of the pandemic, Burke Harris told the Times, to guide both the delivery of prevention resources at the community level and also pragmatic coping mechanisms to individuals (“While dose matters, buffering matters, too,” she said).
But after Floyd’s death on a Minneapolis street a few weeks later, she wrote in her Medium essay that much, much more will also be needed.
“What this moment makes clear… is that addressing health disparities in America through changes to medical practice alone is not enough,” she wrote. “It requires us to address the systemic racism that profoundly hurts our children and our health by immersing them in sustained, dehumanizing trauma…
“It is our collective responsibility to acknowledge and take steps to mitigate the enduring harms of these wrongs.”