XBB.1.5: What you need to know about COVID-19’s ‘Kraken’ variant
Infectious disease expert weighs in on latest variant that is likely behind increase in cases nationwide
As the United States enters a fourth year of COVID-19, there is a new variant called XBB.1.5.
The variant quickly grew in December, from about 1% of cases nationwide to 43% as of Jan. 13, according to data from the Centers for Disease Control and Prevention (CDC).
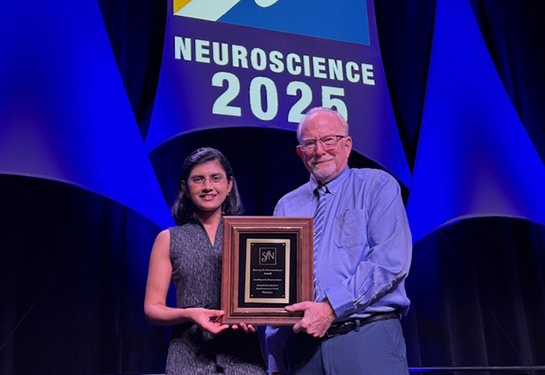
Natascha Tuznik, associate clinical professor of infectious diseases at UC Davis Health, explains what you need to know about XBB.1.5, including symptoms and vaccine efficacy.
How is the XBB.1.5 variant different than previous COVID-19 variants?
XBB.1.5., now dubbed “the Kraken” is the result of two BA.2 omicron variants. Research from John Hopkins shows that this variant has stronger binding capabilities to the target host receptor. That makes it more efficient at spreading and infectious. It has been named the most contagious strain of any COVID-19 variant by the World Health Organization (WHO) thus far.
What are the symptoms of the XBB.1.5 variant? Are they different?
With current available data, the symptoms are similar to the prior strains with no evidence of more severe infection. Recent mutations of COVID-19 have led to less severe disease. This is because the virus must give up something, in this case its ability to do harm, to survive.
How might the recent bivalent vaccine booster work against XBB.1.5?
A perspective from Paul Offit, director of the Vaccine Education Center and attending physician in the Division of Infectious Diseases at Children's Hospital of Philadelphia, showed that the updated bivalent booster may not be more effective as compared the original, monovalent vaccine. This included the new booster not showing an appreciably greater antibody response against the newer omicron variants including BQ.1, BQ1.1, XBB, and XBB.1.5.
This is NOT to say that the vaccine is not effective, just that the bivalent boosters may not be more effective than the original monovalent booster vaccine. That said, the bivalent booster would still be important for people at highest risk of getting severe disease. This includes those ages 65 and older and those who are immunocompromised. Even small, additional increases in antibody production are critically important for them.
Lastly, boosters will continue to help as our antibody production from both natural infection and vaccination decreases over time.
This article was updated January 18 to clarify that it should have referred to “monovalent booster vaccine” instead of “monovalent vaccine” when comparing the updated bivalent booster and the monovalent booster, not the original COVID-19 vaccine.
How can people avoid COVID infection?
These things remain important for people to avoid COVID-19:
- Get vaccinated
- Avoid crowded spaces, especially indoor venues
- Wash your hands frequently
- Consider wearing a mask, especially for people at high risk (for example, immunocompromised)
Learn the do’s and don’ts of mask wearing
Why is it better to avoid getting infected with COVID-19?
There are several reasons it’s important to avoid getting COVID-19. Getting infected puts you at risk of severe illness, potential hospitalization, and death, especially if you are high-risk and unvaccinated. The likelihood of an unvaccinated person dying from COVID-19 has been reported as being between 10-20 times higher than that of a vaccinated person.
In addition, if more people get seriously ill, it could place an unnecessary strain on an already overwhelmed hospital system. Current strains are also better at evading our immune defenses as compared to prior strains. Therefore, your risk of reinfection is higher. Getting infected also puts vulnerable populations at unnecessary risk of infection including severe illness, hospitalization and death.
Last, you could end up with long COVID. There are currently too many unknowns regarding who is more likely to get long COVID, but the risk of developing this chronic condition after infection is very real. Millions of people have developed this and suffer for many months, including time and money lost by the inability to work.
Read more: 9 things we’ve learned about COVID long haulers so far
Could we be nearing the end of COVID?
COVID-19 is unlikely to go away completely. There are still many unknown variables. Virologists wonder whether it will behave like other coronaviruses – many of which cause the common cold. It may end up reappearing seasonally, like most of our viruses do.
In prior epidemics, viruses eventually reach a saturation threshold, meaning most of the population will be or has already been infected. At this point, when the virus has fewer people to infect, the epidemic will decrease naturally.
Hopefully, this will equate to an endemic instead of a pandemic. Endemic is a disease that is still around but at a more manageable level, without causing spikes in deaths, for example. Instead, the disease is more manageable in terms of not overwhelming the system. The hope is that if COVID-19 is not eliminated, it would become more like the common cold.