If you've tried two or more epilepsy medications and still experience seizures, UC Davis Health can help. Additional effective treatments for epilepsy exist, and you deserve the opportunity to learn about and try treatments that are a fit for you. Tell your neurologist you meet the criteria and request a referral for assessment by our multidisciplinary team at the UC Davis Comprehensive Epilepsy Program.
Comprehensive Epilepsy Program
Nationally accredited multidisciplinary care across the lifespan
Child Cured of Epileptic Seizures Thanks to Neurological Surgery – Savon’s Story
Comprehensive Epilepsy Program
You Deserve the Chance to be Seizure Free
Request a ReferralNational experts provide a comprehensive lifespan approach
The multidisciplinary team of specialists in the UC Davis Comprehensive Epilepsy Program are experienced in treating the most complex forms of epilepsy. We offer:
- The region’s most sophisticated complement of intensive neurodiagnostic monitoring and treatment equipment
- The largest staff of epileptologists — specialists in treatment of epilepsy
- Northern California’s only epilepsy program with a comprehensive lifespan approach. We carefully coordinate transition of care among our pediatric and adult specialists as they work together on the same multidisciplinary team. This arrangement ensures maximum treatment safety and patient quality of life across the lifespan.
As one of few programs nationwide to offer this continuity and convenience to patients, our integrated team-based approach also accelerates diagnosis and treatment planning for Northern California patients with unmet neurological needs.
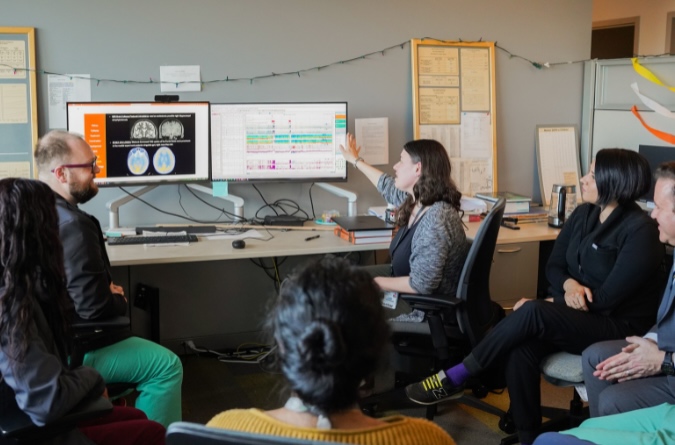

Diagnostic tools and treatments offered at UC Davis
For diagnosis, the Comprehensive Epilepsy Program utilizes continuous EEG and intracranial monitoring or stereo-EEG (SEEG) among its many tools. Patients then may be recommended treatments including medication, responsive neurostimulation (RNS), laser surgery for epilepsy (LITT), a deep brain stimulation (DBS) implant, as well as lifestyle modifications such as the ketogenic diet for epilepsy, or any combination of these and other treatment options.
UC Davis Health is a Level 4 Comprehensive Epilepsy Center
The National Association of Epilepsy Centers (NAEC) has accredited the UC Davis Comprehensive Epilepsy Program for adults and pediatrics as a level 4 epilepsy center, the highest designation available. UC Davis Health is home to the first and only pediatric epilepsy program in inland Northern California to achieve this level accreditation. Only facilities equipped with the most advanced technology and that perform extensive medical, surgical, neuropsychological and psychosocial treatments for epilepsy and other seizure disorders earn NAEC level 4 designation.