Maternal-Fetal Medicine
Maternal Fetal Medicine
Overview
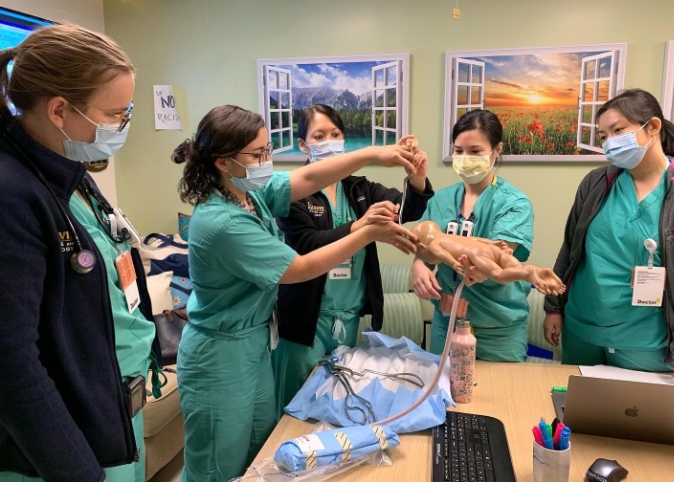
The fellowship training program in Maternal-Fetal Medicine (MFM) at the UC Davis Medical Center is an ACGME-accredited three-year program that includes 24 months of clinical training and 12 months of mentored focused research. There will be one fellow accepted annually into the program, with a total of three fellows. The clinical training includes instruction in all aspects of MFM, including obstetrical, fetal, medical, and surgical complications of pregnancy under the direction of the MFM core faculty. Each fellow will complete 18 months of clinical training in MFM core areas; 6 months of electives, including 2-4 week rotations in NICU, Pathology and Anesthesiology; and 12 months of protected research time. The research experience will have either a basic science research focus or a clinical research focus, with intensive mentorship in either area. Research opportunities are available with mentors at the main campus in Davis, CA as well as the health sciences campus in Sacramento, CA.
The UC Davis Maternal-Fetal Medicine fellowship starts on August 1 and will conclude three years later on July 31.
Program Goals
We aim to train...
- Competent subspecialists who can provide comprehensive and relevant consultation to individuals with complicated pregnancies and their primary pregnancy providers.
- Thoughtful perinatologists able to individualize care to the patient and the resources available to them.
- Leaders in obstetric quality and patient safety.
- Skilled proceduralists, both for diagnostic and therapeutic purposes.
- Effective advocates for the patients, providers, and communities they serve.
- Successful interpreters, communicators, and doers of practice-changing research.

Application Information
Applicants interested in applying for the fellowship training program in Maternal-Fetal Medicine can submit their application through the ERAS website.
The UC Davis Maternal-Fetal Medicine fellowship starts on August 1 and will conclude three years later on July 31.
We will be accepting applications starting in December 2024 for the 2026-2027 academic year. The program will adhere to the SMFM common program dates.
- Application deadline: Monday, April 28, 2025
- Interview invites will be sent: Monday, May 19, 2025
- Interview dates: August 13 and August 27, 2025
In addition to the ERAS application, applicants are requested to send copies of CREOG scores directly to Shea Hazarian. This program requires a minimum of three letters of recommendation. If a rotation was completed at a fetal surgery center and that letter is not included as one of the letters of recommendation, please send that to Shea as well.
Individuals interested in obtaining additional information should contact:
Shea Hazarian, M.P.H.
916-734-1039
sahazarian@ucdavis.edu
Training Location
The primary location for the program is at the UC Davis Medical Center in Sacramento. The Division of Maternal-Fetal Medicine also provides services in the Northern California region that extends north to the Oregon border, south to the San Joaquin Valley, east to Reno, Nevada, and west to the Bay Area. All Division members are on the faculty of the UC Davis School of Medicine.

-
Leanna Sudhof, M.D.
View profilearrow_forwardAssistant Professor
Fellowship Program DirectorLeanna Sudhof is a maternal-fetal medicine specialist who chose this field because she loves the complexity of pregnancy care and wants to be able to help at what is often a particularly vulnerable time. She has special interests in preterm birth, multiple gestation, substance use disorders in the perinatal period, perinatal mental health, and postpartum hemorrhage. She also has expertise in prenatal diagnosis, including amniocentesis and chorionic villus sampling, and other fetal procedures.
-
Herman Locsin Hedriana, M.D.
View profilearrow_forwardProfessor
Division Chief of Maternal-Fetal MedicineHerman Hedriana returned to UC Davis’s Maternal-Fetal Medicine division in Obstetrics and Gynecology in March 2018. He was an Assistant Professor in Residence from July 1994 through June 1998 and for over 19 years, he has been Volunteer Clinical Faculty. Hedriana's main focus is premature birth risk assessment including preterm labor evaluation and effective use of antenatal corticosteroids. He feels patient safety, welfare, and their right to information comes first. He has been an active volunteer for March of Dimes for 15 years, involved in prematurity prevention, health care disparities, and healthcare policies involving different communities in California.
-
Nina Boe, M.D.
View profilearrow_forwardClinical Professor
Nina Boe's clinical interests include prenatal diagnosis, pregestational and gestational diabetes, preeclampsia, and complications with twin gestations. Her research activities focus on improved screening procedures for diabetes in pregnancy.
-

Zahabiya Chithiwala, M.D., M.H.S.
Associate Physician
Zahabiya Chithiwala received a B.S. in Physiological Sciences from the University of California, Los Angeles and a M.H.S. in Biochemistry and Molecular Biology, Reproductive and Cancer Biology from Johns Hopkins Bloomberg School of Public Health. She received her M.D. from Drexel University College of Medicine in 2017. She completed her residency in Obstetrics and Gynecology at the University of California, Davis in 2021.
-

Shannon Clark, M.D.
View profilearrow_forwardAssistant Clinical Professor
Shannon Clark is board certified in Family Medicine and Psychiatry and completed a fellowship in Clinical Obstetrics. Her specialty interests focus on the care of pregnant women with mental illness or substance abuse. Clark also created and runs a weekly medication management and support group for women with mood disorders from pre-conception through one-year postpartum. The group setting aims to promote the development and delivery of health infants by treating and supporting the emotional well-being of the mother as an adjunct to prenatal and postpartum care.
-
Nancy Field, M.D.
View profilearrow_forwardClinical Professor
Nancy Field's areas of interest include management of diabetic pregnancies, medical complications and fetal growth abnormalities during pregnancy, and fetal sonography. Her research currently focuses on outcomes in diabetic pregnancies.
-

Amelia McLennan, M.D.
View Profilearrow_forwardAssociate Clinical Professor
Director, Fetal Care and Treatment CenterAmelia McLennan joined the Maternal-Fetal Medicine division after completing her fellowship at Columbia University in New York, NY. She offers care for women with a range of high-risk medical, surgical, and fetal conditions during pregnancy. She has special clinical interest in ultrasound, prenatal diagnosis, genetic testing, multiple gestations, and fetal therapy.
-

Lihong Mo, M.D., Ph.D.
Assistant Professor
Lihong Mo is a Maternal-Fetal Medicine physician with a dedicated focus on providing comprehensive care for patients carrying high-risk pregnancies. Her clinical interests include hypertensive disorder of pregnancy, multiple gestations, preterm birth prevention, and the integration of technology-driven maternal care. Mo’s research focuses on advancing perinatal research via data science.
-
Carolina Reyes, M.D.
View profilearrow_forwardAssociate Clinical Professor
Carolina Reyes joined the department of Obstetrics and Gynecology in 2019. She has extensive academic experience teaching and providing care in southern California and Washington, DC. Her research focuses on testing strategies to improve the practice of perinatal care during the intrapartum and postpartum period when women are at highest risk for cardiovascular complications of pregnancy. Reyes enjoys working with residents and fellows while helping patients and their families grow.
-
Krishna Singh, M.D.
View profilearrow_forwardDirector, UC Davis Prenatal Diagnosis Center
Assistant Clinical ProfessorKrishna Singh joined the department of Obstetrics and Gynecology at the University of California, Davis, School of Medicine in 2020. She is triple board certified in Obstetrics and Gynecology, Maternal Fetal Medicine, and Medical Genetics and Genomics. She has brought her expertise in Prenatal Genetics to the Division of Maternal-Fetal Medicine and the Fetal Treatment Center. Singh has specialty in diagnostic evaluation and advanced molecular testing of fetuses and adults with rare genetic disorders.
-
Véronique Taché, M.D.
View profilearrow_forwardClinical Professor
Residency Program DirectorVéronique Taché specializes in taking care of women with high-risk pregnancies. Her clinical interests include fetal growth abnormalities, multiples and higher order multiples, prevention of preterm birth, maternal coagulation disorders and endocrine disorders.
-

Elisa Zhang, Ph.D.
View profilearrow_forwardAssistant Professor
Elisa Zhang started her research laboratory at UC Davis in July 2024 in the Departments of Obstetrics and Gynecology and Physiology and Membrane Biology. She received her Ph.D. in molecular and cellular biology from UC Berkeley and conducted her postdoctoral research at the Stanford University School of Medicine as an A.P. Giannini Fellow. Her lab studies uterine, placental, and pregnancy biology. Her research focuses on how the uterus regenerates itself during the menstrual cycle and following injuries like C-sections, as well as how the placenta develops and functions at the maternal-fetal interface.
-
Paige Cleek, M.S., C.G.C.
Licensed Certified Genetic Counselor
-

Noura Osman, M.S., L.C.G.C.
Licensed Certified Genetic Counselor
Noura Osman practices communicating with preconception/prenatal patients about genetic diagnoses in a tailored manner that attempts to foster psychological resilience and facilitate decision-making during challenging times. Being raised in Egypt and Canada, she began to appreciate human diversity and its intersection with genetic disease and communication. She has a special interest in the psychotherapeutic components of genetics and strives to have meaningful conversations with her patients to allow them to feel emotionally enriched and empowered. Noura enjoys collaborating on research projects that aim to improve genetic healthcare for vulnerable populations as well as research that attempts to delineate novel phenotypes for rare genetic conditions.
-

Laila Rhee, M.S., C.G.C.
View profilearrow_forwardLicensed Certified Genetic Counselor
Laila Rhee is a genetic counselor specializing in prenatal counseling primarily to women and families with high risk pregnancies. She has a special interest in fetal congenital heart disorders, neuromuscular disorders and infertility. Respecting autonomy and rights of the patient, she wants to provide genetic information and support so that patients make informed decisions about their medical care and make the best possible adjustment for their family.
Diversity
The UC Davis Gynecologic Oncology Fellowship values having trainees with a diversity of thought, experience, and perspective. Care is taken to interview candidates who come from a variety of backgrounds. The Office of Graduate Medical Education supports Inclusive Excellence and Equity with all fellowship and residency programs to create a climate of belonging and equity.
Sacramento is one of the most ethnically and socially diverse cities in America, and the large rural catchment area of UC Davis Health includes many critical access areas serving patients with complex needs and low resources. Throughout your training here you will learn to care for patients from around the world and prepare yourself to provide quality care to those who need it.