Varicocele
Expert Care for Enlarged Testicular Veins
Making an appointment
You can schedule a visit to discuss your diagnosis by calling 916-734-2222.
A varicocele is defined as dilation of the veins that drain the testicle. It is typically diagnosed during a physical exam of the scrotum. Varicoceles are common and it is estimated that about 15% of men are living with a varicocele. However, in men who suffer from infertility, it is much more common.
A varicocele is graded according to the following scale:
- Grade I (felt only during Valsalva maneuver)
- Grade II (felt in the standing position without Valsalva maneuver)
- Grade III (visible)
- It is causing pain.
- It is thought to be contributing to impairment of sperm quantity and function, possibly leading to infertility.
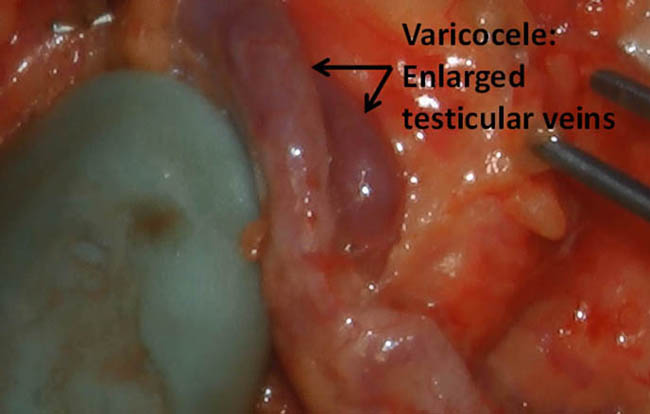
What a Varicocele Looks Like
Frequently Asked Questions (FAQs)
It is easiest to think of the varicocele as a varicose vein of the scrotum. These enlarged veins can lead to accumulation of blood in the scrotum around the testicle leading to an achy testicular pain that typically worsens with activity and prolonged standing. This pain is usually mild to moderate but can be anywhere from annoying to debilitating to some patients. Treating the varicocele with surgery, if done on the appropriate candidate patient, can lead to resolution or decrease in pain in 60-80% of patients (it depends on what particular study you look at). There may be other reasons why a patient will have testicular or scrotal pain however, and therefore it is important patients are counseled appropriately prior to considering treatment for their varicocele.
Similar to how a varicocele can cause pain, it is thought that a “back-up” of blood in the testicle may harm sperm. While the exact mechanism isn’t fully understood, possible effects include DNA damage to sperm, increased heat stress and reduced blood flow to the testicle.
Typically, a varicocele is felt on an examination in a patient being evaluated for pain or infertility. With an infertility diagnosis, and occasionally in patients with pain only, we will generally recommend a semen analysis to assess the patient’s fertility potential. A semen analysis will usually report on a man’s sperm count, sperm movement, semen volume and other factors that are thought to be important to measure a man’s fertility potential. Depending on the situation (partner age, other modifiable clinical factors, etc.) we may recommend treating the varicocele. Based on the interpretation of many studies done on varicocele repair, patients can expect to have an improvement in their sperm count and movement, although there are exceptions with some patients improving more than others and the very rare patient having a slight decline in semen quality.
The methods used to treat a varicocele are noted below. In most patients the safest and most effective way of treating a varicocele is the microscopic approach (listed below as microscopic sub-inguinal). It is associated with the least amount of unwanted side effects, such as hydrocele (fluid collection around the testicle), and leads to fewer recurrences. Other ways of treating a varicocele may be better for certain patients. We specialize in the microscopic approach (microsurgical varicocelectomy).
|
Technique |
Artery Preserved |
Hydrocele (%) |
Recurrence (%) |
Potential for |
|
* Microscopic sub- inguinal Retroperitoneal Conventional inguinal Laparoscopic Embolization |
Yes No No Yes Yes |
0 7 3-30 12 0-12% |
1-2 15-25 5-15 5-15 2-15 |
No No No Yes Yes |
We perform this surgery under general anesthesia using an operating microscope. We begin by making a 2-3 cm incision in the lower abdomen on the side(s) that is affected.
Through this incision, we bring up the spermatic cord (structure containing the arteries, veins and other structures coming from the testicle). After the spermatic cord is identified, we begin by searching for the veins we will tie and cut to treat the varicocele.
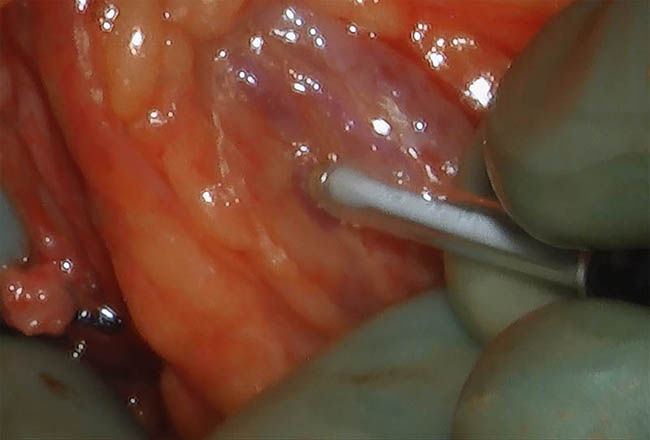
A microvascular doppler is used to listen to the testicular artery so that it is more easily identified and safely dissected away from the veins that are to be cut.
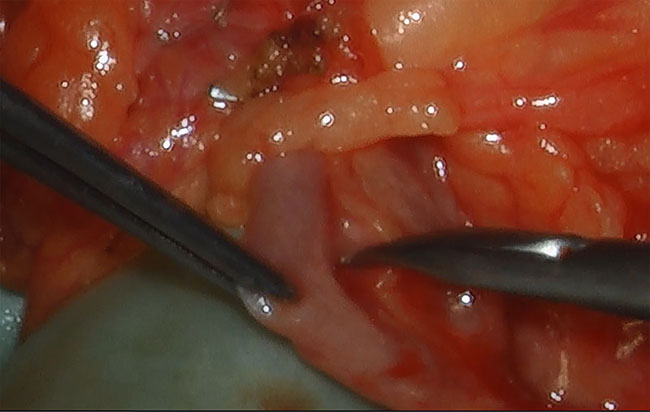
Fine microsurgical instruments are used to isolate the veins away from critical structures such as the testicular artery.
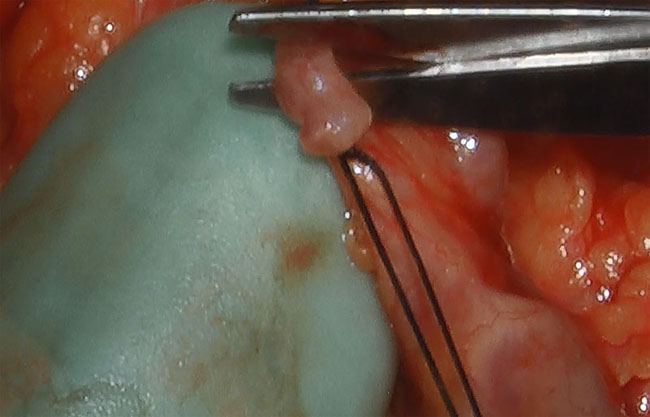
The enlarged veins are tied off to seal them.
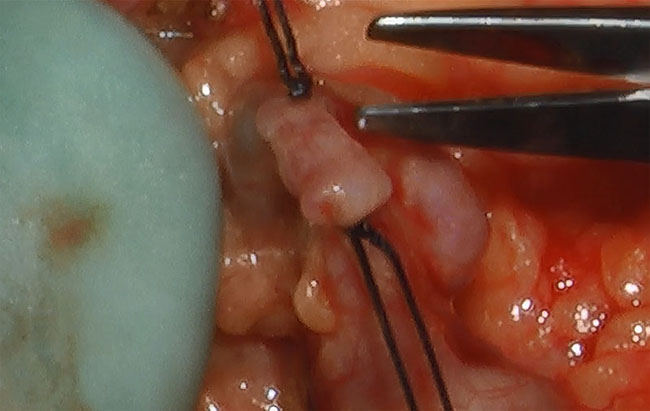
Fine scissors are used to cut the veins.