A little-known respiratory virus, HMPV, surged this spring. What you need to know
Young children, those who have weakened immune systems and older adults most at risk of serious illness from human metapneumovirus
If you came down with a respiratory infection in the spring and it wasn’t influenza (flu), COVID-19 or RSV, it may have been a virus you’ve never heard of.
That’s because cases of human metapneumovirus, or HMPV, surged across the U.S. in March.
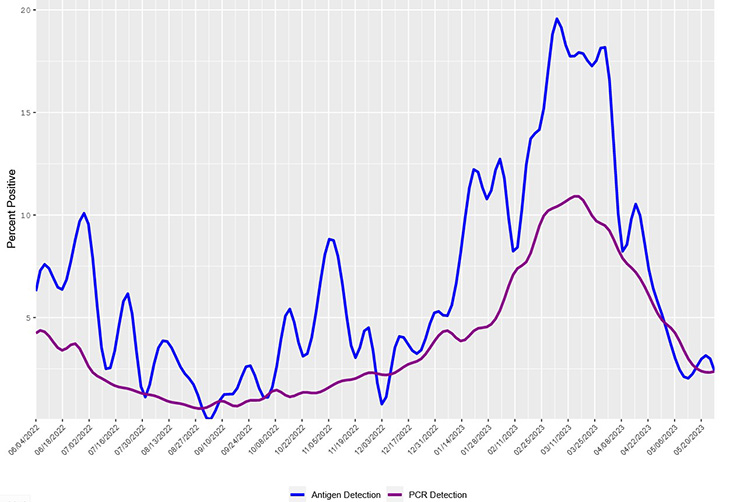
According to the Centers for Disease Control and Prevention (CDC), 19.6% of antigen tests and 10.9% of PCR tests for HMPV were positive in early and mid-March. The numbers are about 36% higher than before the pandemic.
The virus is seasonal, like the annual flu. In the United States, HMPV infections begin circulating in winter and last through spring. And the good news is that levels have dropped.
“HMPV is not something most people need to worry about. It’s essentially another cause of the common cold,” said Larissa May, a professor of emergency medicine and an expert in public health and testing for infectious diseases.
Why you likely won’t know if you had HMPV
There are no antiviral drugs specifically for HMPV like there are for the flu and COVID-19. Which is why physicians usually don’t test for it.
“The treatment of mild or moderate viral upper respiratory infections is supportive no matter what the viral cause, so we generally do not recommend testing for most outpatients,” said Dean Blumberg, chief of pediatric infectious diseases.
Treatment is the same as a cold — lots of fluids to prevent dehydration, decongestants to reduce congestion, and pain relievers like ibuprofen and other NSAIDs for body aches.
May noted that it’s a common misunderstanding that antibiotics can help. “They will not help you recover from HMPV because antibiotics do not work against viruses,” May said.
The virus was first discovered in 2001. HMPV is in the Pneumoviridae family, along with the more commonly known respiratory syncytial virus or RSV.
Although in most people, HMPV causes a mild cold, it may cause more severe disease resulting in hospitalization for some.”—Dean Blumberg, chief of pediatric infectious diseases
“HMPV causes disease very similar to RSV,” Blumberg said. “This includes upper respiratory symptoms that sometimes progress to pneumonia or bronchiolitis and wheezing. Although in most people, HMPV causes a mild cold, it may cause more severe disease resulting in hospitalization for some.”
The virus can cause upper and lower respiratory disease in people of all ages but is most common in children, especially those under 5 years of age.
According to Blumberg, infants and young children less than 2 years of age are most at risk for complications like bronchiolitis. “Children born prematurely, with heart or lung disease, or weakened immune systems are at higher risk for severe disease,” Blumberg said.
Others at higher risk are people who have had organ transplants, those with cancer, those who take long-term steroids and those over 75 years of age.
UC Davis test detects over 20 respiratory viruses
Currently, there are no home tests for HMPV. For hospitalized or high-risk patients with respiratory illness, UC Davis has a combined test that can help diagnose multiple viruses and bacteria that commonly cause respiratory disease.
Similar to a PCR COVID-19 test, the multiplex respiratory panel uses a nasal swab specimen. It can detect non-COVID coronavirus, parainfluenza, Flu A and B, RSV, C. pneumoniae, M. pneumoniae, rhinovirus, enterovirus, and adenovirus. It can also differentiate sub-types of these pathogens.
“The panel lets us look at all the common causes of respiratory disease all in one test. In practice, it is used when common pathogens like flu A and B, SARS-CoV-2 and RSV are not detected with other routine PCR platforms, and there's a critical need to know what else could be causing the respiratory infection,” said Nam Tran, a professor and senior director of clinical pathology at UC Davis Health.
May noted, “Testing isn’t generally needed for people who don’t have complications. They are only needed for certain patients, like those who are immunosuppressed or admitted to the hospital with a respiratory infection.”
Because testing is primarily conducted in a hospital setting, the actual number of HPMV infections every year is unknown. A 2020 study published in The Lancet found that there were an estimated 14.2 million cases of HPMV globally in children younger than 5 years old.
Symptoms and how to protect yourself
Symptoms of HMPV are similar to a cold and include a sore throat, chest congestion and a cough, nasal congestion and sometimes a fever.
“HMPV may be prevented by respiratory hygiene, such as avoiding and covering coughs and good hand hygiene — washing hands after contact with potentially infectious secretions or surfaces,” Blumberg said.
If you have cold-like symptoms, to prevent spreading the virus you should:
- cover your mouth and nose when coughing and sneezing
- wash your hands frequently with soap and water for at least 20 seconds
- avoid sharing cups and eating utensils
- refrain from kissing others
- stay at home when sick
When to see a doctor
You should call your doctor if you or your child has one or more of these conditions:
- difficulty breathing
- chest pain
- difficulty keeping fluids down
- symptoms that last more than 10 days
- symptoms that are severe or unusual
- if your child is younger than 3 months of age and has a fever or is lethargic
You should also call your doctor right away if you are at high risk for serious complications and get symptoms such as fever, chills, and muscle or body aches.
Resources

